Want to Increase Suicide Risk? Use Cannabis!
A new meta-analysis addresses the increase in risk we have chosen to ignore.
I'm a huge square. I've never smoked a cigarette, and I've never had an alcoholic “drink” in its entirety. I've never used a recreational drug. This includes cannabis. I do have a medical cannabis card, and used it to get a 20:1 CBD:THC tablet…once. It didn't work well enough for my psoriatic arthritis pain, and I gave up on it.
The medicalization of cannabis was the path that advocates chose to help get a formerly illegal drug to be legal. I'm no fan of the war on drugs, and its associated collateral damage. But turning cannabis into a medicine? Absent research on medical risks and benefits? Longtime readers will realize I've actually written about this topic before… this newsletter is up to over 950 articles and podcasts!
When it comes to PTSD, cannabis has limited evidence:
Cannabis also has additional risks, such as dementia and early death:
As I wrote just last week, it is also a leading driver of depersonalization symptoms:
Today, we’re diving into a specific risk as it relates to cannabis: the risk of suicidal ideation, behavior, and, heavens forbid, completed suicide.
I know, I'm a literal buzz kill! Dear readers, this is my sweet spot.
Cannabis gets you high. Some people use cannabis for a reasons that are valid but not medical. They use it to enjoy themselves, which comes with risks:
Perhaps unsurprisingly, those with a greater number of substance-using peers are more likely to report enhancement motives, and enhancement motives are endorsed more often on the weekend, as well as on days when people report greater use. Importantly, only weekend enhancement motives were associated with cannabis-related problems, suggesting that a subset of people may seek enjoyment from cannabis use at the expense of other, possibly more important or meaningful, activities on the weekend.1
Which is true of many of the activities we do for fun. Nobody is out there demanding that binge drinking come with a prescription. We haven't tried to medicalize skydiving, or disappointing dates, or excellent dates with problematic lovers, or going to the shooting range with your friends. None of these things involves a prescription from a doctor. People use cannabis for reasons that they understand—because getting high feels good—and, because of a very successful, political agenda—we end up trying to shoehorn that experience into a medical model. If you can't tell already, I think that's a dumb idea.
They use it socially:
Key hallmarks of social use motives include the desire to “celebrate a special occasion with friends” or because it “makes social gatherings more fun.”
They use it to expand their minds:
“I use cannabis so I can know myself better” or “…it helps me be more creative and original.”
People smoke cannabis enhance, relax, forget their cares, or distract themselves from their problems. These are understandable uses of a substance, but it's important to remember that this isn't medicine when used in this way. Even Tylenol can be dangerous when we use too much of it. Not everything that is biologically active is a medicine or medicinal. Many biologically active agents create a potent change in your brain also come with risks.
Cannabis and Suicide Risk
Like, for example, the risk of killing oneself at higher rates than would otherwise occur.
In a recent systematic review and meta-analysis of 25 studies2 called:
The role of depression in the relationship between cannabis use and suicidal behaviours: A systematic review and meta-analysis
Maviel and colleagues evaluated 25 papers that allowed the authors to control for depression severity when evaluating suicidal ideation:
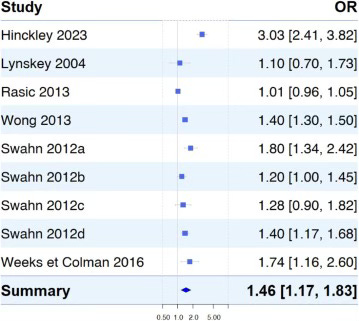
Among adolescents, cannabis use was associated with suicidal ideation (OR = 1.46 [1.17, 1.83]) and suicide attempts (OR = 2.17 [1.56, 3.03]) in studies adjusting for depression.
Among adults, cannabis use was associated with suicidal ideation (OR = 1.78 [1.28, 2.46]) in studies adjusting for depression.
My readers will remember that the vertical line in that Forest Plot, right in the middle, is the “equipoise line.” Aka if the sample crosses the line, it’s not different from chance. The diamond on the very bottom has a “width”—which represents the confidence interval—and as long as it doesn't cross the vertical line, the overall data suggests that something, in this case thinking about suicide, even when you take depression in to account—happens more when you smoke cannabis.
But “worry” about this result, because while the risk of thinking about suicide is higher by a modest degree, the risk of attempting suicide is higher by an even larger degree, in adolescents:
For suicide attempts among adolescent who use cannabis, the pooled OR was 1.85 [1.37, 2.5] (Fig. 2). Heterogeneity was high (I² = 95.1 % [93.1 %, 96.5 %]).
Like most observational and non-controlled data, this was not a slam dunk:
The Egger’s test (p = 0.013) and the funnel plot showed asymmetry, indicating probable publication bias.
And even if we were looking at individual studies, one could miss this increased risk effect:
12 out of 25 studies found no association between cannabis use and suicidality after adjustment for depression.
Cannabis is riskier in youth than in adults, and one of those risks is being more suicidal. Another is psychosis. In older adults, it’s dementia. Cannabis is not safe.
How Unsafe Are We Talking?
However, for a moment of perspective, there are other fun things young people do that are similarly not “healthy.” Let’s take one of the leading pastimes of youth: staying up late. It turns out, this is when more people end their lives than at other times of the 24-hour day:
The primary results from this study were that 1) 20% of suicides occurred at night and 2) when accounting for the proportion of the population that is awake at each given hour, suicide is much more likely to occur at night then during the morning, afternoon or evening hours.
The authors pulled this data from a database of all the deaths by suicide:
n = 35,332 documented suicides. The ATUS is a database maintained by the US Bureau of Labor Statistics (BLS) and is an annual survey that assesses a range of activities across the 24-h day in a representative sample of Americans.
The data included the time of death. It’s way riskier to stay up late than it is to smoke cannabis:
The maximum incident rate was at 2:00–2:59h (16.3%). Hour-by-hour observed values differed from those that would be expected by chance (p < 0.0001), and when 6-h blocks were examined, the observed frequency at night was 3.6 times higher than would be expected by chance (p < 0.0001).3
Not everything that's fun is healthy. In fact, some very fun things are a really bad idea when done chronically.
It's worth having a sense of the risks we’re taking on, and having an appropriate public health attitude towards risk that allows us to have rational conversations with our patients, if we are healers, or make better decisions for ourselves, if we're the ones putting the risks on our own shoulders.
Don't smoke cannabis, don't stay up late, don't get in the car, don't do anything risky. Or, pick the risks you're facing in a manner that is in keeping with your values and personal risk tolerance.
Thanks for reading!
Where Can I Get Help? Radial!
I have a day job—when I’m not writing this newsletter— as the Chief Medical Officer of a company called Radial.
If you (or a loved one) are looking for relief from Depression, OCD, Anxiety, PTSD, Bipolar Disorder, or even a compassionate assessment of depersonalization/derealization disorder, feel free to explore care with Radial.
Radial offers the most advanced mental health care.
Radial has physical locations in Midtown Manhattan, Brooklyn, NY; Myrtle Beach, SC; La Jolla, CA; and more, with additional locations coming soon. We currently provide telehealth services in 20 states and are also screening participants for research trials globally.
Gex, K. S., Gückel, T., Wilson, J., Ladd, B. O., & Lee, C. M. (2024). Why people use cannabis and why it matters: A narrative review. Current Addiction Reports, 11(6), 1045-1054
Maviel, G. M., Somma, C., Davisse-Paturet, C., Airagnes, G., & Melchior, M. (2025). The role of depression in the relationship between cannabis use and suicidal behaviours: A systematic review and meta-analysis. Drug and Alcohol Dependence, 112714.
Perlis, M. L., Grandner, M. A., Chakravorty, S., Bernert, R. A., Brown, G. K., & Thase, M. E. (2016). Suicide and sleep: is it a bad thing to be awake when reason sleeps?. Sleep medicine reviews, 29, 101-107.