Schizophrenia Is More Dangerous Than A Car Crash, and Treating it Saves Lives
Challenging truths about a challenging illness, in the wake of the RADAR trial.
The Frontier Psychiatrist's newsletter? It is what you are reading. It’s a health-themed publication written by Owen Scott Muir, M.D. This is a brief detour from my recent series on medications, many of which have a critical slant. Those include Risperidone, Depakote, Geodon, Ambien, Prozac, Xanax, Klonopin, Lurasidone, Olanzapine, Zulranolone, Benzos, Caffeine, Semeglutide, Lamotrigine, Cocaine, Xylazine, Lithium, dextromethorphan/bupropion and Adderall, etc. I write this all by myself every day. Consider subscribing. (the paywall starts 5 weeks back, and there are 360something articles back there). It makes a horrible or awesome gift, depending on your friend circle.
I also get paid more money by Amazon if my readers buy stuff now, like, for example, my favorite book about mental illness—or this tea I drink daily. I also encourage you to send me this coffee maker— or, more realistically, to anyone else.
Today, I address what happens when schizophrenia is not treated, even if it is. It has high morbidity and mortality, a problem that medications address. Effectively. Not without costs, but the best data suggests treatment is better than no treatment for most people.
I’m going to cut to the chase briefly, and if you or a family member want to read a great book on treatment with antipsychotic medicine, I’d recommend this one. Jeff Leiberman, M.D., has been …controversial… of late. However, there is no denying his role in understanding schizophrenia and its treatment, and his book on the topic is worth a read or listen, called a Malady of the Mind.
Psychotic. We use the word commonly in chit-chat to denote something is bad. Unreasonable. Wrong. Deranged. Nothing is beguiling about the word. It is a thing to deny in oneself— “I am not psychotic!”
Understanding Psychosis
Some people don’t get that luxury. Some people are honest-to-goodness psychotic. Most of us do not know what that means. Some of us do, and some smaller portions are blessed with the ability to spend time on both sides of that psychotic equation. I will define the term:
Psychosis refers to a collection of symptoms that affect the mind, where there has been some loss of contact with reality. During an episode of psychosis, a person’s thoughts and perceptions are disrupted and they may have difficulty recognizing what is real and what is not1.
The most common illness we associate with psychosis is schizophrenia. Psychosis can occur with depression, bipolar disorder, and other maladies. Depression and mania are mood states; we refer to these mixed with psychotic symptoms as affective disorders in psychiatry. A brief grammar note, brought to you by Grammarly, a tool I use and—sadly—am not paid to promote2:
Is affective just another word for effective? Are the two words similar and entangled in the way the verbs affect and effect are? No, affective is not just another word for effective. And affective and effective are not derived from the verbs affect and effect. They come from the nouns affect and effect.
There is a difference in the literature—and in the lives of patients—when it comes to illnesses that have affective psychosis and non-affective psychosis. Much of the anti-psychiatry crowd focuses on affective disorders and argues about the side effects of those treatments. Less attention is paid to non-affective psychosis because It’s not as compelling an argument. These are challenging illnesses either way and are associated with significant morbidity—impairments in life—and mortality—early death.
“Uncured of Worse”: 1937.
As far back as 1937, authors noted the grim prospects in the long-term course of schizophrenia (in this context, I’m referring to largely “non-affective psychosis” —where the delusions or hallucinations are not tied to mood episodes):
Of the 100 cases, 66% were uncured or worse after the lapse of 6-10 years, with persisting process symptoms or in a defective state after the course had run; 13% were improved, 4% were cured with defects, and 17% were completely cured.3
“The Prognosis is Poor”: 2010
By 2010, with decades of more data, the conclusion was much the same—schizophrenia sucks, even compared to other admittedly bad illnesses:
Our 26-year longitudinal study and other longitudinal studies confirm older views that outcome for schizophrenia, while showing some variation for different schizophrenia patients, is still significantly poorer than that for other psychiatric disorders.4
A large NIMH follow-up study with 2 to 10 years of time following patients from a first episode that required hospitalization demonstrated:
The sample showed substantial functional impairment and levels of symptoms, with only about 20% of the sample demonstrating a good outcome…
The “not-good” outcomes looked like this:
78% of the sample suffered a relapse, 38% attempted suicide and 24% had episodes of major affective illness.5
Beyond Psychiatric Problems?
We tend to focus on the role of bad psychiatric outcomes as psychiatrists. Still, the medical outcomes are similarly troubling, including high smoking rates, metabolic syndrome, heart disease, HIV, Hepatitis C, and other medical illnesses.6 Overall, this leads to an extremely disheartening finding: having schizophrenia is an illness that takes a tremendous toll on the individual and their family and leads to early death and disability at unacceptably high rates:
Persons with schizophrenia have an exceptionally short life expectancy. High mortality is found in all age groups, resulting in a life expectancy of approximately 20 years below that of the general population. Evidence suggests that persons with schizophrenia may not have seen the same improvement in life expectancy as the general population during the past decades. Thus, the mortality gap not only persists but may actually have increased.7
Comparisons are useful, and if we look at HIV after the introduction of HAART (Highly Active Anti-Retroviral Therapy), we find:
HIV-related mortality decreased from 6.5 to 1.3 per 100,000 population (80% decrease, p = 0.0115). New HIV diagnoses declined from 702 to 238 cases (66% decrease; p = 0.0004) with a consequent estimated decline in HIV incident cases from 632 to 368 cases per year (42% decrease; p = 0.0003).8
And if we compare that to schizophrenia, in the largest meta-analysis I could find, we find:
The mortality risk for patients with schizophrenia was 1249 per 100 000 … (95% CI, 1029-1469)9
Psychosis is Bad Compared to Other Bad Things
The mortality from schizophrenia is 19,215% higher than from pre-HAART HIV infection and 96,076% higher than from HIV with HAART treatment.
If you had to choose between HIV and schizophrenia, HIV is safer—with or without treatment.
To make the point even more clearly, even having a car crash only has a 0.77% fatality rate, or 770/100,000.10
If you had to choose between a car crash and schizophrenia, the car crash is safer.
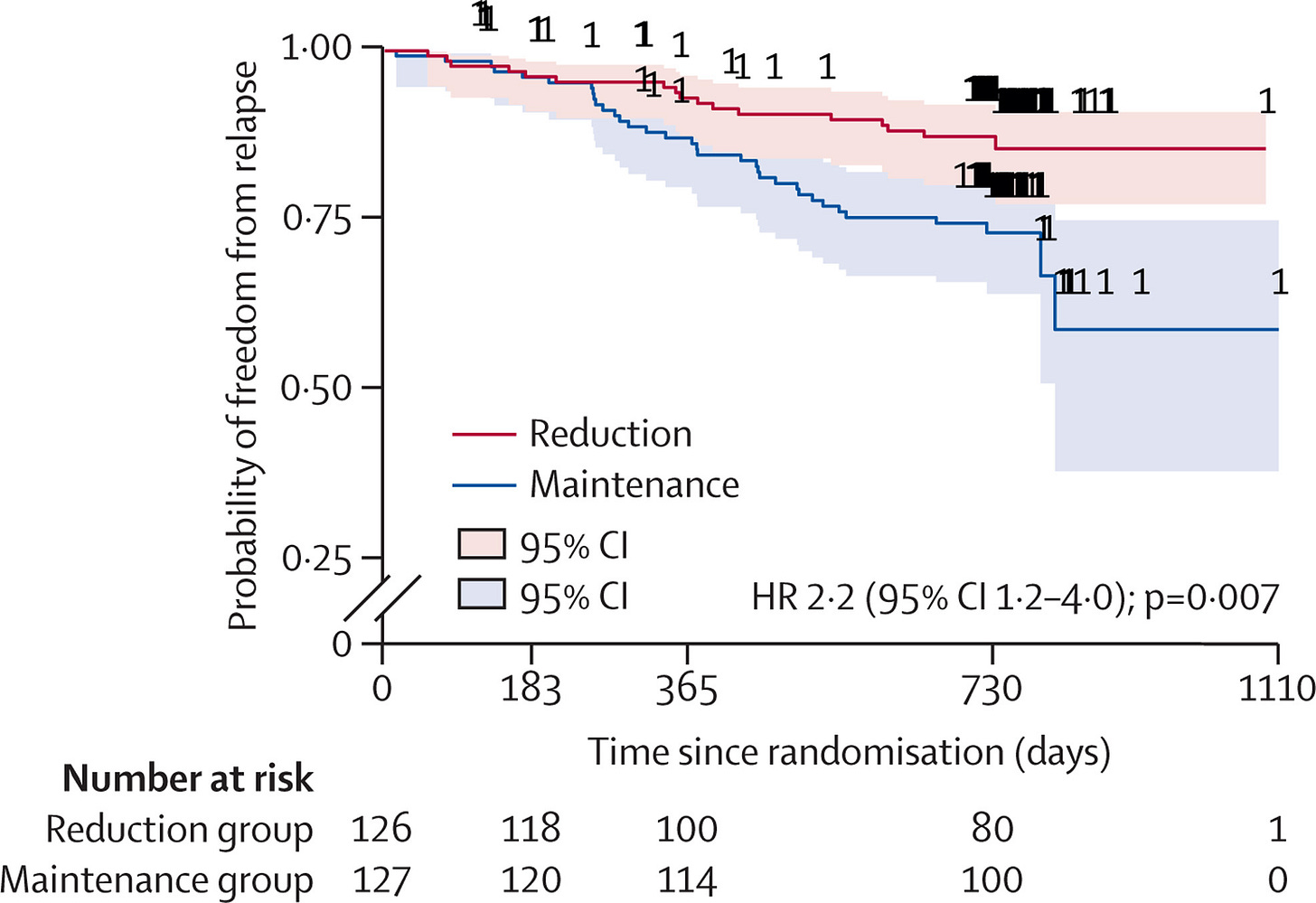
Those outcomes are not good enough. Schizophrenia is impairing and dangerous to your life, especially if untreated. Other psychiatric illnesses are also. Psychiatric medications can modify this risk to your life in the right direction, even with those risks. Tapering them, as we saw in the RADAR trial11 (lead-authored by a critical psychiatrist, published in the Lancet just this week12), doesn’t make it better:
At 2-year follow-up, a gradual, supported process of antipsychotic dose reduction had no effect on social functioning.
And, further, made it worse:
here were 93 serious adverse events in the reduction group affecting 49 individuals, mainly comprising admission for a mental health relapse, and 64 in the maintenance group, relating to 29 individuals.
It includes twice as many deaths. In a research study, this is a huge deal. The way to look at this is the probability of relapsing is bad, and it’s statistically more likely and with more than double likelihood if you were randomized to a taper protocol.
Antipsychotic Medication Saves Lives. It has Burdens. These Choices are Difficult.
We need to do better, but the haters are incorrect. We have done better than nothing, even with imperfect tools, even when examined by those who have an axe to grind with those very tools. Treatment of schizophrenia saves lives.
Stay Humble,
Faced with Suffering,
and Carry On
Hola At Ya Author, Grammarly. I’m accepting sponsorships. I am also responsible for more unique words than 99% of your users. I’m in the 97% for total words generated last month, which means professional writers are doing less than me, and I have nine other jobs.
Langfeldt, G. (1937). The prognosis in schizophrenia and the factors influencing the course of the disease. Acta Psychiatrica et Neurologica (KjøBenhavn), Suppl. XIII, 228.
Jobe, T. H., & Harrow, M. (2010). Schizophrenia Course, Long-Term Outcome, Recovery, and Prognosis. Current Directions in Psychological Science. https://doi.org/10.1177/0963721410378034
Breier A, Schreiber JL, Dyer J, Pickar D. National Institute of Mental Health Longitudinal Study of Chronic Schizophrenia: Prognosis and Predictors of Outcome. Arch Gen Psychiatry. 1991;48(3):239–246. doi:10.1001/archpsyc.1991.01810270051007
Goff, D. C., Cather, C., Evins, A. E., Henderson, D. C., Freudenreich, O., Copeland, P. M., ... & Sacks, F. M. (2005). Medical morbidity and mortality in schizophrenia: guidelines for psychiatrists. Journal of Clinical Psychiatry, 66(2), 183-194.
Laursen, T. M., Nordentoft, M., & Mortensen, P. B. (2014). Excess Early Mortality in Schizophrenia. https://doi.org/10.1146/annurev-clinpsy-032813-153657
Montaner, S. G., Lima, V. D., Harrigan, P. R., Lourenço, L., Yip, B., Nosyk, B., Wood, E., Kerr, T., Shannon, K., Moore, D., Hogg, R. S., Barrios, R., Gilbert, M., Krajden, M., Gustafson, R., Daly, P., & Kendall, P. (2014). Expansion of HAART Coverage Is Associated with Sustained Decreases in HIV/AIDS Morbidity, Mortality and HIV Transmission: The “HIV Treatment as Prevention” Experience in a Canadian Setting. PLOS ONE, 9(2), e87872. https://doi.org/10.1371/journal.pone.0087872
Khan A, Faucett J, Morrison S, Brown WA. Comparative Mortality Risk in Adult Patients With Schizophrenia, Depression, Bipolar Disorder, Anxiety Disorders, and Attention-Deficit/Hyperactivity Disorder Participating in Psychopharmacology Clinical Trials. JAMA Psychiatry. 2013;70(10):1091–1099. doi:10.1001/jamapsychiatry.2013.149
Moncrieff, J., Lewis, G., Freemantle, N., Johnson, S., E Barnes, T. R., Morant, N., Pinfold, V., Hunter, R., Kent, L. J., Smith, R., Darton, K., Horne, R., Crellin, N. E., Cooper, R. E., Marston, L., & Priebe, S. (2019). Protocol: Randomised controlled trial of gradual antipsychotic reduction and discontinuation in people with schizophrenia and related disorders: The RADAR trial (Research into Antipsychotic Discontinuation and Reduction). BMJ Open, 9(11). https://doi.org/10.1136/bmjopen-2019-030912
Moncrieff, J., Crellin, N., Stansfeld, J., Cooper, R., Marston, L., Freemantle, N., Lewis, G., Hunter, R., Johnson, S., Barnes, T., Morant, N., Pinfold, V., Smith, R., Kent, L., Darton, K., Long, M., Horowitz, M., Horne, R., Vickerstaff, V., . . . Priebe, S. (2023). Antipsychotic dose reduction and discontinuation versus maintenance treatment in people with schizophrenia and other recurrent psychotic disorders in England (the RADAR trial): An open, parallel-group, randomised controlled trial. The Lancet Psychiatry. https://doi.org/10.1016/S2215-0366(23)00258-4



My heart goes out to people living with schizophrenia - I've learned so much about the challenges. Agreed with you on treatment - if I'm in a car with a significant risk of crashing and it's a question of "when" not "if", I'd rather live in the universe where that car has a seatbelt and other safety features rather than the beater car from the 80's with suspect seatbelts.
Thank you.