Readers of this newsletter are familiar with the machine learning revolution. I can't stop writing about it. It's very exciting. It's already turning into treatments for neuropsychiatric conditions, and today, I get to tell you about the FDA-cleared PRISM system. Welcome to The Frontier Psychiatrists, a daily-enough health-themed publication.
One of the major bummers of having symptoms of PTSD is that people keep wanting to talk about mental health. For people who have experienced significant trauma, talking about it is often the last thing they want to do. It would be fantastic if there were treatments that didn't require you to talk about an awful thing. They would still need to work! Traditional psychotherapies for PTSD are effective, and they require having conversations that desensitize you to your experience of trauma, but they're doing that by modulating your brain. It can be challenging to think about embarking on this when your traumatic experiences are causing distress! Even if therapy could help, you might avoid doing it in the first place.
After years of diligent research using functional magnetic resonance imaging synchronized to EEG brainwave analysis, the team at GrayMatters Health created an algorithm that can identify changes in the brain's fear center, known as the amygdala.
The non-brand name for this modality? It’s long: Amygdala-derived-EEG-fMRI-pattern neurofeedback.1
What does it look like? A video game you play with your brain. I made a quick video:
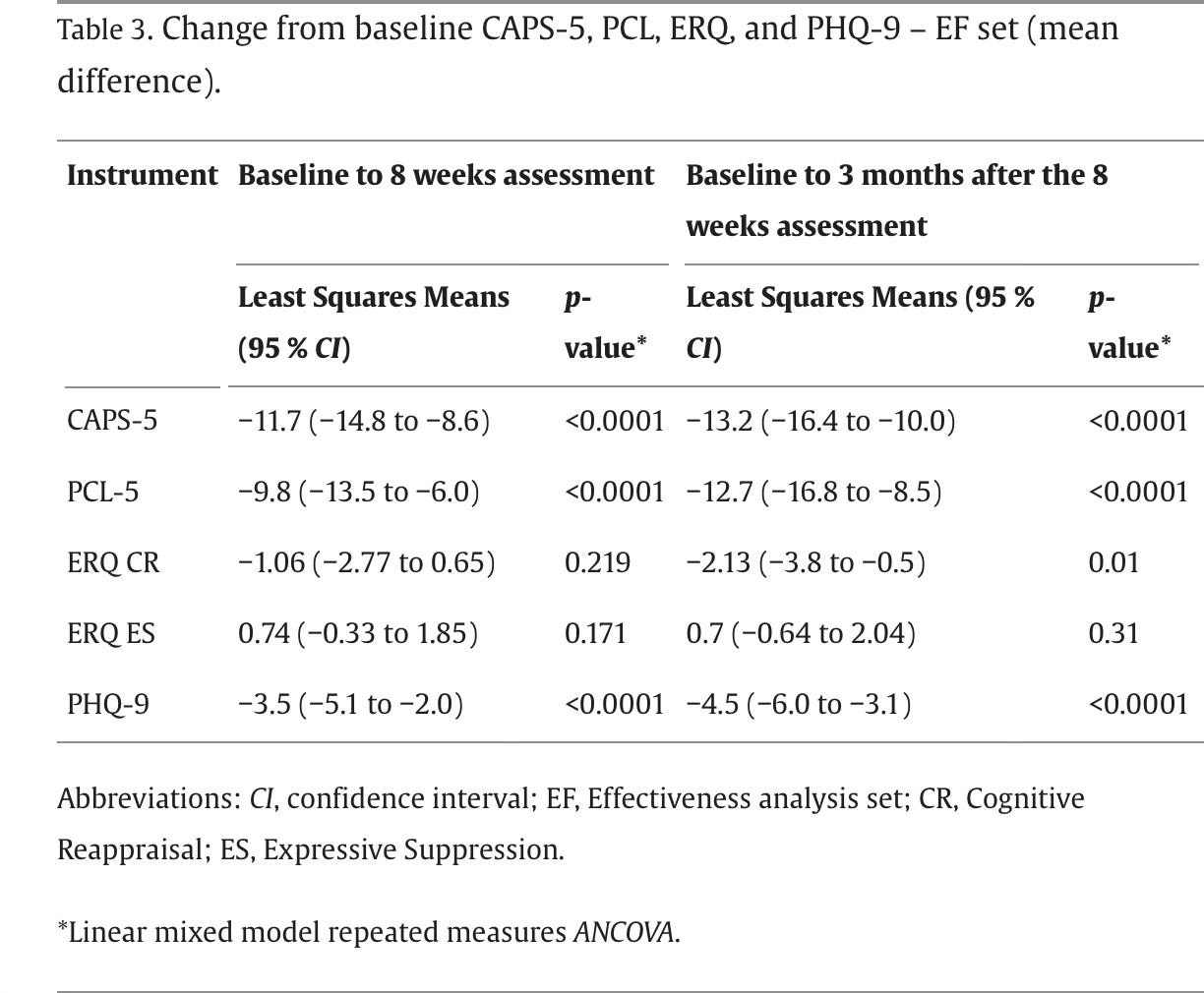
The treatment consists of sitting in a chair, looking at a computer screen, and getting people in the video game to sit down and stop complaining. When PRISM reads your brain, calming your amygdala down, the video game moves in the right direction. This repeats throughout five cycles per session. This process, repeated in 15 sessions in their pivotal trial, led to remarkable relief of symptoms in many participants:
This trial used a “within-subjects” comparison design, so there was no placebo; each person's performance was compared to themselves at different time points. This is a robust statistical design, similar to the “mirror-image” designs championed by John Kane for studying Long-Acting Injectable antipsychotics.2
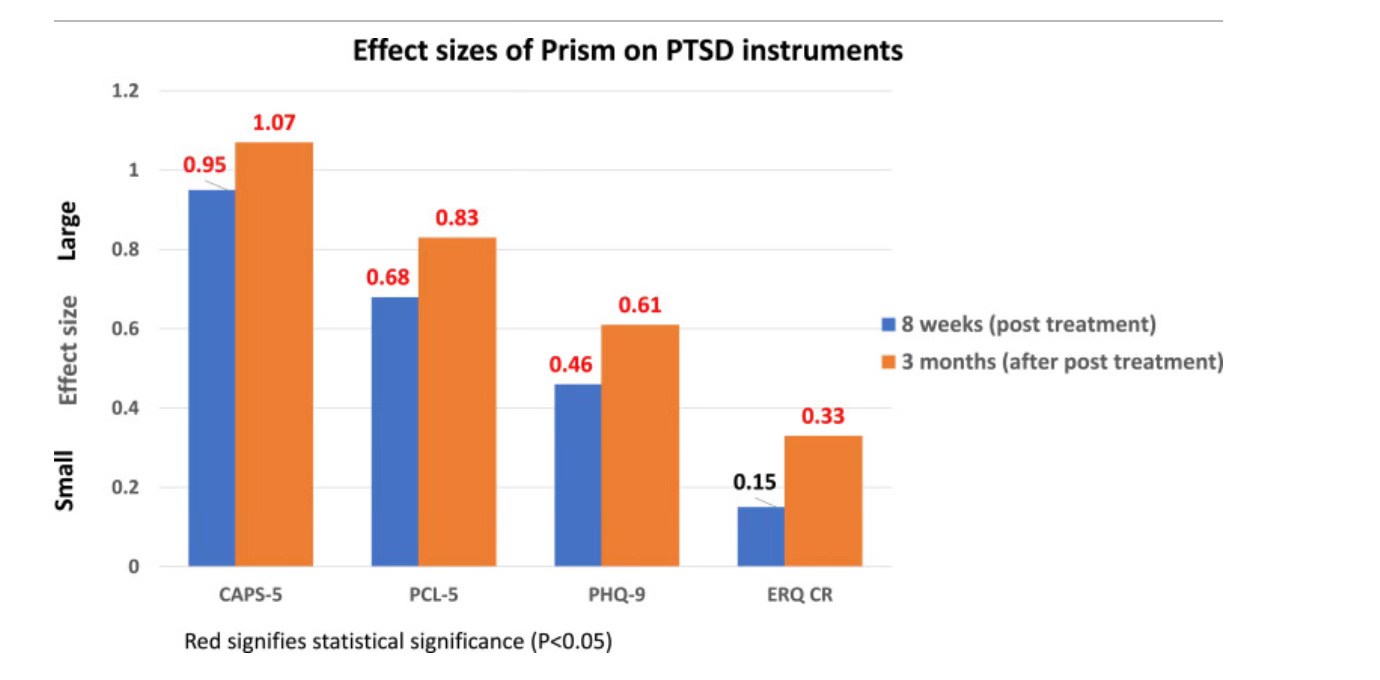
I have written about the importance of effect sizes on many occasions. Look what we have in this trial:
Yes, on the CAPS-5, we find an effect size of 0.95— which improves to 1.07 three months after the treatment course is completed. It’s worth noting that this is a larger effect size than cited in my team’s review on MDMA (as submitted to the FDA by Lykos as part of MDMA-AT):
Phase III clinical trials led by the Multidisciplinary Association for Psychedelic Studies (MAPS) have shown that MDMA-assisted psychotherapy has an effect size of d = 0.7–0.91, up to 2–3 times higher than the effect sizes of existing antidepressant treatments.3
As noted earlier this week, that data is now resting on the unsteady foundation of retracted publications and an FDA denial. Even if you believe MDMA-AT is 100% as good as claimed? PRISM treatment, although not directly compared, is similarly potent in the PTSD population studied, with a superior effect size of 1.07 at three months of follow up.
There is hope for PTSD. In PRISM treatment, you sit silently, not talking about your trauma, concentrating in a way that teaches your brain to heal. It’s fast, already in use at our clinic, Fermata, in Brooklyn, and vastly less time-consuming than MDMA-AT’s proposed protocol.
There is trauma therapy we don’t have to talk about…and it still works better than existing treatments.
A reminder— I have a book! It’s about drugs, and how much I don’t use them, and why that is. Inessential Pharmacology. (amazon link)
Fruchter, E., Goldenthal, N., Adler, L. A., Gross, R., Harel, E. V., Deutsch, L., ... & Marmar, C. R. (2024). Amygdala-derived-EEG-fMRI-pattern neurofeedback for the treatment of chronic post-traumatic stress disorder. A prospective, multicenter, multinational study evaluating clinical efficacy. Psychiatry Research, 333, 115711.
Kishimoto, T., Nitta, M., Borenstein, M., Kane, J. M., & Correll, C. U. (2013). Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. The Journal of clinical psychiatry, 74(10), 10539.
Shinozuka, K., Tabaac, B. J., Arenas, A., Beutler, B. D., Cherian, K., Evans, V. D., ... & Muir, O. S. (2024). Psychedelic Therapy: A Primer for Primary Care Clinicians—3, 4-Methylenedioxy-methamphetamine (MDMA). American Journal of Therapeutics, 31(2), e141-e154.




Neurofeedback tech is pretty neat. I do think this looks promising. But not everyone realizes that fda approval for technology isn’t based on efficacy. And they might not realize the clinical study you’re citing is based on 60-ish subjects, 88% of whom were white. Might be nice to see the real life data on this.
> Traditional psychotherapies for PTSD are effective
Many people who are furious that the FDA didn't approve MDMA don't acknowledge this enough (see the article below -- 65% experience some symptom reduction "in a national sample of veterans").
However, many people who are happy the FDA didn't approve MDMA oversell the efficacy of current treatments (this same article shows "only 36% experienced clinically significant improvement"). Anyway, point taken -- effect sizes matter!
https://pubmed.ncbi.nlm.nih.gov/30785007/