Nutritional Ketosis for Bipolar Disorder
On world bipolar day, a diet that may be a treatment reviewed
Welcome to The Frontier Psychiatrists! It’s a daily health-themed newsletter. March 30th is World Bipolar Day. Thus, some on-theme content for my dear readers. It’s also, for the curious, Doctor’s Day, and, with grim irony, The Grass is Always Browner on the Other Side of the Fence Day.
I review the data on a hopeful intervention in bipolar disorder. I’ve written about having that very illness here. I’m not alone in coming out, as a physician, with bipolar. Stigma delenda est.
Can a Diet Do Anything for a Serious Mental Illness?
What loaded questions I asked myself! Let’s define “nutritional ketosis” first, because although the mechanism is “changing what you eat,” calling it a diet puts it in the same category as numerous fads, scams, and minor changes. That is not what I am talking about with a ketogenic diet.
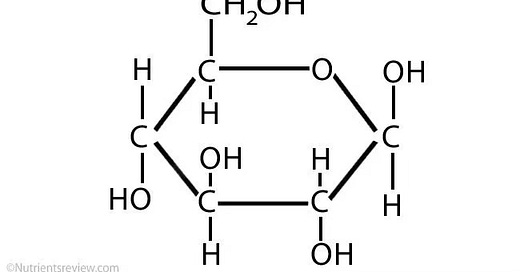
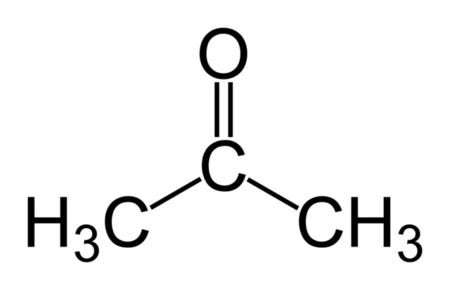
And, because of course, I’m going to do some organic chemistry education. A ketone body is a carbon-containing molecule:
There are three ketone bodies, as featured above, produced by the liver. They are acetoacetate, beta-hydroxybutyrate, and acetone. These compounds are used in healthy individuals to provide energy to the cells of the body when glucose is running low in the blood.
They are an alternative fuel source for human biology. In those diagrams, a single line indicates a molecular bond—the sharing of electrons. A double line indicates a “double bond” where two pairs of electrons are shared. One of the things left out of these drawings by convention is that at every point of inflection, there is an omitted “C” for the carbon molecules that form the backbone of biology. It was decided a long time ago that we would not like to waste our time as chemistry teachers drawing endless carbon molecules, so they are implied. In the Acetone above, there is oxygen up top and three carbon molecules are implied at each of the points connected by the peaked lines. This diagram includes them;
So, we are often abbreviating the carbons—and their attached hydrogen molecules—in the drawings of organic molecules that I post!
Deep, nerdy breath. Onward.
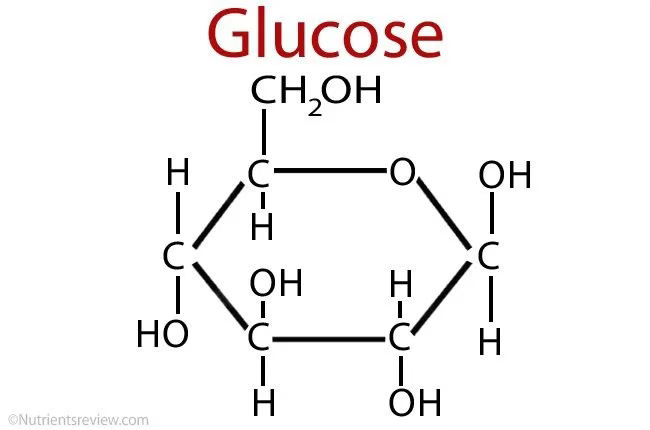
The body—and brain—usually run on glucose. Glucose looks like this:
When we are running low on glucose we still can’t let our body run out of energy. So we have a backup. The brain can power its cells with ketone bodies instead of glucose. Thus, by strategically eating foods that force the body into ketosis, we can flip a powerful biological switch. We aren’t starving—but absent carbohydrates, we run out of glucose, and burn through all the backup stored in our liver, and start powering the body with this different fuel source.
Some diets you can half-ass and still get the result you want. This is not the case with a ketogenic diet. To be in a state of depleted glucose such that the body repurposes its molecular machinery to run on ketone bodies instead? This is an all-or-nothing choice. You can eat a “sort of keto” diet—but this will not create the change in biology necessary.
Thus, ketogenic diets are VERY strict to deprive the body of all the glucose it would otherwise use to power itself, and force it into the generation of ketone bodies because they have the potency to change biology.
It’s less than 50 net grams of carbs a day—which is a tiny amount.
Starting with a disorder we will all agree is both profoundly biological and in the brain—but not bipolar disorder—we have epilepsy. In two landmark studies in 1998, a ketogenic diet led to dramatic changes in seizure frequency in youth with treatment-refractory epilepsy:
In 1998, a multicenter study was conducted in 51 children with drug-resistant epilepsy1 47% of children remained on a diet for a year. 43% of them were seizure-free, 39% controlled 50–90% of seizures, and 17% did not respond.
A Hopkins trial of 150 children found similar outcomes that same year.2 Nutritional Ketosis was a real biological intervention in epilepsy, and a comprehensive review of its use in that disorder is in the footnotes.3
The logical jump to bipolar disorder requires a slight cognitive hop-skip-and-a-jump. Bipolar disorder would need to be understood as a disorder that had its basis in the biology of the brain. What if a mood episode wasn’t because you were “just an assh*le?” What if…it was a real disorder? One that involved biology?
I’m being a little glib. Bipolar disorder is often the brunt of jokes, including very funny ones. One of the issues with research into bipolar disorder, I’m convinced, is that the people most motivated to do it, like your author, are very much at risk of being belittled and dismissed for having the very illness they are invested in cures for.
To quote The Onion, in it’s masterpiece on the topic:
“Depression is a serious and complex mental illness, but there’s no reason we can’t solve it tonight—there’s nothing holding us back,” said head researcher Dr. Gavin Rowe, trembling euphorically as he mentioned that he felt “unstoppable” and had been working on the problem for the past 49 hours straight. “We’ll just run a few experiments in the next half hour, develop a medication, nail down some dosages, and get rid of depression once and for all. That’s it. Christ, we’re finally thinking clearly!”
Sometimes-manic individuals—no matter how brilliant or correct about the science—are going to be dismissed more often than others when they have great new insights. The raised eyebrows around those with manic-depressive illness are warranted, we bipolar sufferers will be the first to agree (when not in a mood episode). However, it doesn’t change the fact that sometimes-manic people are sometimes-correct about new science.
This science is more likely to be dismissed as flights of fancy by the rest of you. This is both understandable and regrettable.
One of the leading proponents of Nutritional Ketosis is Chris Palmer, M.D. He describes his “long experience” with “mental illness” in this interview, and has written a phenomenal book, Brain Energy (affiliate link). You will notice, he doesn’t say which mental illness—and such is stigma. We can’t even say it out loud for fear of being dismissed when we are trying to change the perspectives of the world around that disorder. I don’t know if Chris has bipolar disorder. I know, for sure, I do—and given how people respond, I don’t begrudge anyone their privacy.
Dr. Palmer has advanced a hypothesis, that the mitochondria in the cells of our brain are the core of dysfunction in both epilepsy, as treated with nutritional ketosis above, and in illnesses like bipolar disorder and schizophrenia. I am going to restrain myself from doing more science education, and skip to the empirical question—what is the evidence that profoundly changing your diet, such that your brain and its mitochondria use a different fuel source, can treat bipolar disorder?
A pilot study published this year by colleagues at Stanford4 has hopeful, if problematic, results. Over 4 months, in 23 subjects, the following was observed:
Clinical Global Impressions severity [CGI-S] of mental illness assessments show an average improvement of 31 % (baseline 3.6 +/- 1.0, p < 0.001). The proportion of participants who were in the recovery state at baseline. In the adherent group, 100 % were in the recovered state by the end of our study.
The issue, of course, is this is an incredibly hard treatment to blind, and non-adherence impacts the outcomes of the intervention. At the same time, thoughtful scientists will imagine there may be differences between individuals with bipolar disorder generally and those with bipolar disorder who are capable of adhering to a ketogenic diet for 4 months. The data set continues:
Overall, for both bipolar and schizophrenia populations, 43 % (p < 0.02) of participants achieved recovery during the study (50 % for those adherent (p < 0.01), and 33 % for those semi–adherent). In participants with baseline symptoms (of at least mild illness or greater severity), 79 % (p < 0.001) achieved a marked improvement (defined as 1–point CGI change), with 92 % (p < 0.001) for those adherent and 50 % for those who were semi–adherent.
Dr. Ede, a leader in the field, has recently published a retrospective chart review which is a strong argument for more research, as well—with the caveats about methodology right up front (edited for easy reading to exclude the standard deviations):
Three [of 31] patients were unable to adhere to the diet for >14 days and were excluded from the final analysis. …The mean Hamilton Depression Rating Scale scores from 25.4 to 7.7 P < 0.001, and the Montgomery-Åsberg Depression Rating Scale from 29.6 to 10.1, P < 0.001. Among the 10 patients with schizoaffective illness, the mean of the Positive and Negative Syndrome Scale (PANSS) scores improved from 91.4 to 49.3, P < 0.001.5
The data, I will grant, is thin on the ground. The potential for individuals who have suffered tremendously is similarly a major opportunity. Unlike other scientific breakthroughs, no one needs to deal with a Pharma company to deploy this intervention. It’s meat, veggies, and not sugar or bread or rice or corn or other stables of the modern diet. Georgia Ede, M.D. has a new book on the Ketogenic Diet, available here (affiliate link)—this is the most up-to-date instruction manual.
The methodological issues are significant, I will note. Self-serving studies beset by survivor bias, hucksterism, and regression to the mean are a regular target of my snark, and that of other colleagues like Al Lewis in his classic on health economics, “Why No One Believes the Numbers” (affiliate link). Nutritional Ketosis is VERY hard to blind and hard to stick with for many people. It’s not impossible, however. One could imagine a study in which, after everyone enrolled got on a ketogenic diet, they were given a Sucralose shake every day of follow-up, and randomized to the time point at which it was switched out for real sugar. People would likely notice getting knocked out of ketosis, but that design has been used in studies in both aripiprazole LAI and lamotrigine, historically.
Until we have well-blinded trials, we should maintain skepticism about how good of an option nutritional ketosis is going to be, and for whom. When we only evaluate people who stick with a treatment, we risk significant bias. When we gloss over the difficulty of sticking with a regimen that could be helpful, we risk losing track of those who couldn’t do it and needed the help too. To dismiss emerging science that could relieve suffering because it hasn’t all been completed yet? We also diminish both the suffering and the efforts of those who are onto something.
I want to close this column by highlighting an organization that has done a remarkable amount to push science forward—Metabolic Mind. It is doing a huge lift to get the word out and fund the work. No story about this effort would be complete without mentioning my friends Jan and Matt Baszucki. Matt lives with bipolar disorder, tried everything to get well, and although other things were helpful-ish, nothing has had the impact of the Ketogenic Diet. His mother, Jan, is in the role many family members are in—she wants her child to be well. She saw the difference with Nutritional Ketosis. She also co-runs a foundation with her husband, The Baszucki Group. Her efforts have been relentless. Parents know their kids. They know the difference between “eh, better?” and “well.”
On World Bipolar Day, a deep thank you to the families of those with bipolar disorder everywhere. Without you, none of the progress would be possible. To close with a moment of levity, again, the Onion, from its “What Your Therapist is Actually Thinking While You are Talking” slide show:
Thanks for reading—and have a euthymic day!
Prior articles on bipolar disorder and its treatments include Geodon, Ambien, Xanax, Klonopin, Lurasidone, Olanzapine, Benzos, Caffeine, Semeglutide, Lamotrigine, Lithium, dextromethorphan/bupropion and Adderall, Abilify II, Abilify III, Abilify, frightening articles about Tardive Dyskinesia, Reasonable Accommodations, this interview on the Soft White Underbelly, a podcast on the open letter to my own bipolar disorder, articles on the risks of bad sleep, a chat with Dr. Drew on the topic, is Bipolar Disorder a Circadian Rhythm Disorder, and even a discount card for your medications. And more, including this classic:
Depakote
The Frontier Psychiatrists is this newsletter. Owen Muir, M.D. writes it, and it is a satirical take, personal, or both, on health-related issues of the day. Dr. Muir is a child and adult psychiatrist. T…
Vining, E.P.; Freeman, J.M.; Ballaban-Gil, K.; Camfield, C.S.; Camfield, P.R.; Holmes, G.L.; Shinnar, S.; Shuman, R.; Trevathan, E.; Wheless, J.W. A multicenter study of the efficacy of the ketogenic diet. Arch. Neurol. 1998, 55, 1433–1437
Freeman, J.M.; Vining, E.P.; Pillas, D.J.; Pyzik, P.L.; Casey, J.C.; Kelly, L.M. The efficacy of the ketogenic diet 1998: A prospective evaluation of intervention in 150 children. Pediatrics 1998, 102, 1358–1363.
Sethi, S., Wakeham, D., Ketter, T., Hooshmand, F., Bjorstead, J., Richards, B., ... & Saslow, L. (2024). Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Psychiatry Research, 115866.
Danan, A., Westman, E. C., Saslow, L. R., & Ede, G. (2022). The ketogenic diet for refractory mental illness: a retrospective analysis of 31 inpatients. Frontiers in psychiatry, 13, 951376.






A terrific piece, Dr. Muir. We'll put this on our web site as a less biased and clearer-eyed view than the one that reigns in our parts. Thanks for the nice shout-out at the end. Matt remains in full remission, no episodes, no symptoms, tapered off lithium a year ago, continuing the taper for the other meds. Questions: What would it take for an unconventional psychiatrist like yourself to make patients aware of this intervention? Given it is well established for weight loss and treatment and prevention of diabetes, should psychiatrists make their patients aware even if the evidence in psychiatry is still emerging? Should psychiatrists be responsible for treating the metabolic syndrome the meds they prescribe induce? I am not convinced that a blinded trial is ethical. If you put a member of this vulnerable population through the trouble of going on a ketogenic diet for three of four months, it feels nasty to undo their progress with a glucose shake every day. And then you would have to blind them to their ketone levels, which could be quite tricky. It may be more important to map metabolic and psychiatric effects to ketone levels. We are trying to make sure our studies use ecological momentary assessments, especially for bipolar, to catch daily mood shifts. I'll pose to our network if there have been blinded keto trials in epilepsy. Anyway, excellent piece. Bravo.
Is the brain energy book worth reading as a MD or its for too broad an audience?