Lithium: The Depressing Case of Misrepresented Monitoring Data I
A Frontier Psychiatrists' Guest Series!
One of the most exciting things about The Frontier Psychiatrists—a daily-enough health-themed newsletter? It has grown beyond anything I could have imagined. I have transitioned slowly from “writer” to author and from author to editor. In the process, the newsletter has been thrilled to welcome a series of guest columnists. You may remember Alex from his previous hit article, “That is So Random.” Alex is a pen name, but he is a real Ph.D in physics. What comes next is the first of a five-part epic on Lithium monitoring. If you need a lithium primer, I’d suggest checking out the chapter in my book, Inessential Pharmacology. (amazon affiliate link). I’d also nudge you to leave a review. You will likely enjoy this series with that data in hand. It’s thrilling to have this newsletter become a living, breathing, collective undertaking befitting the plural after the word psychiatrist.
…you are up!I was quite excited to learn about the recently published book called “The Lithium Handbook” by Jonathan Meyer and Stephen Stahl [1]. Lithium prescriptions seem to be slowly decreasing [2], [3] despite the evidence showing lithium as one of the (if not the) most effective bipolar maintenance treatments [3], [4], [5]. Lithium needs all the proponents it can get.
I found a series of webinars by Dr Meyer based on the handbook. I watched the section on lithium therapeutic monitoring and immediately felt down, frustrated and a tad angry. For some reason, my way of venting is to spend a day searching through my personal Zotero catalogue1 of references (other citation managers are available) and writing an article attempting to inform and educate. I’m not sure how it got to the point where I, a physicist with absolutely no training in psychiatry, am trying to inform the public about interesting facets of lithium pharmacokinetics, but here we are.
Let’s get straight to it.
Every story has a beginning, an end… and then another end?
At around the ten-minute mark in the webinar video: “Baseline monitoring and dosing of lithium”, the following plot is presented comparing the pharmacokinetic curves for different types of lithium tablets from a single dose.

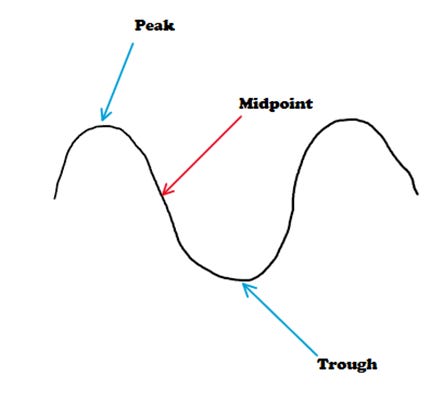
The plot mentions “12-hour trough values” with an arrow pointing to a part of the elimination curve that is around halfway between the max and minimum concentration. This is not the trough. It is approximately the midpoint.
The trough is the lowest value of the wave, or, in the case of the lithium pharmacokinetic curve, the lowest serum concentration—which is just after the next dose of lithium is taken (assuming it will take a little bit of time for lithium to be absorbed into the bloodstream).
I’m not entirely sure why this simple error is made, but I do know it has been made in the academic literature, too [6] [7]. I hypothesize that historically most patients were on a Multiple Daily Dosing (MDD) regimen - usually twice daily. This would mean the 12-hour lithium serum levels would have been taken just before the next dose. These are essentially trough levels. When Single Daily Dosing (SDD) started to be used more frequently (making the 12-hour level the midpoint), I guess the terminology stayed around?
I find this quite worrying because if some clinicians think the trough is the midpoint and others think it is the lowest concentration value, one can imagine miscommunication happening very easily. A patient could be put in danger. It is not outside the realms of possibility that an accidentally taken 24-hour level is interpreted as a 12-hour level.
But this isn’t why I felt down listening to Dr Meyer’s webinar…
A cliffhanger for the end of part I! Stay tuned for part II! Please follow
on substack, or even subscribe to his newsletter![1] J. M. Meyer and S. M. Stahl, The Lithium Handbook: Stahl’s Handbooks. in Stahl’s Essential Psychopharmacology Handbooks. Cambridge: Cambridge University Press, 2023. doi: 10.1017/9781009225069.
[2] X. Pérez de Mendiola, D. Hidalgo-Mazzei, E. Vieta, and A. González-Pinto, “Overview of lithium’s use: a nationwide survey,” Int. J. Bipolar Disord., vol. 9, p. 10, Mar. 2021, doi: 10.1186/s40345-020-00215-z.
[3] L. V. Kessing, “Why is lithium [not] the drug of choice for bipolar disorder? a controversy between science and clinical practice,” Int. J. Bipolar Disord., vol. 12, no. 1, p. 3, Jan. 2024, doi: 10.1186/s40345-023-00322-7.
[4] E. Severus et al., “Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis,” Int. J. Bipolar Disord., vol. 2, p. 15, Dec. 2014, doi: 10.1186/s40345-014-0015-8.
[5] C. Volkmann, T. Bschor, and S. Köhler, “Lithium Treatment Over the Lifespan in Bipolar Disorders,” Front. Psychiatry, vol. 11, p. 377, May 2020, doi: 10.3389/fpsyt.2020.00377.
[6] T. S. Schoot, T. H. J. Molmans, K. P. Grootens, and A. P. M. Kerckhoffs, “Systematic review and practical guideline for the prevention and management of the renal side effects of lithium therapy,” Eur. Neuropsychopharmacol., vol. 31, pp. 16–32, Feb. 2020, doi: 10.1016/j.euroneuro.2019.11.006.
[7] W. A. Nolen et al., “What is the optimal serum level for lithium in the maintenance treatment of bipolar disorder? A systematic review and recommendations from the ISBD/IGSLI Task Force on treatment with lithium,” Bipolar Disord., vol. 21, no. 5, pp. 394–409, Aug. 2019, doi: 10.1111/bdi.12805.
Alex is from the UK. thus the spelling.






This is why we write.
This was insanely confusing for me as an intern in psychiatry. Definitely a dumb vestige that lingers due to our laziness.