Does Lithium Prevent Suicide in Bipolar Disorder? An Existential Guide.
As told by a psychiatrist who's been there.
“Don’t Kill Yourself, with Lithium!”
I am going to make the case that the above tagline is an appropriate slogan for lithium. This article will be a comprehensive guide to the prescribing, effects, and side effects of lithium.
I have a more radical agenda, however than a guide to appropriate dosing. I argue that treating symptoms—according to the data on lithium—isn't the best job for the medical discipline of psychiatry. When we focus only on symptoms, we might miss out on the difference between suffering and living. Lithium is the most dramatic example of this paradox. Although it's a mildly effective symptom reducer, it's a wildly effective way to stay alive. The fact that these are different outcomes of the same treatment raises existential questions.
As a note, this article talks in detail about suicidality and reducing the risk of suicide completion, but if you're feeling suicidal, or someone you love is, 988 is the number to call. It exists. It works. Help is helpful. There are options to get out of the hole, and more every day.
What is Lithium?
Lithium is the third element on the periodic table. It’s salt. It has three protons. It has three electrons. It has four neutrons. It’s pretty straightforward from a chemistry perspective.
It’s also an awesome Nirvana song:
This element, and its various forms, can be very potent in bipolar disorder. I have bipolar disorder. I've written about it before. I will write about it again.
I’ve taken lithium myself. I don’t take lithium anymore. I wasn’t lucky enough to be in the “lithium responsive” cohort.
Bipolar disorder probably has different subtypes—we use the scientific term “endophenotypes” for these, to confuse non-scientists. And “lithium responsive bipolar disorder” might be one of these “endophenotypes” of bipolar disorder.
It’s even been the topic of a few excellent podcasts… like this one by Radiolab1:
Why Lithium in Bipolar Disorder?
Lithium: so you don't kill yourself!
Lithium is effective in managing bipolar disorder symptoms, and more specifically preventing relapse to mania and acute mania and reducing cycle frequency over time. It also protects your neurons from dying, as this review in Bipolar Disorders (2009) points out:
Enhancing neuroprotection (which directly involves neurotrophic effects) is a therapeutic strategy intended to slow or halt the progression of neuronal loss, thus producing long-term benefits by favorably influencing outcomes and preventing either the onset of disease or clinical decline.
Further:
It is important to emphasize that lithium has already demonstrated diverse molecular effects, reversing well-described pathophysiological changes such as increased oxidative stress, programmed cell death (apoptosis), inflammation, environmental stress, glial dysfunction, neurotrophic factor dysfunction, excitotoxicity, mitochondrial and endoplasmic reticulum (ER) dysfunction, and disruption in epigenetic mechanisms.
There are many good reasons the lightest metal on the periodic table is remarkable—and is much more than “a mood stabilizer.”
My Opinion:
Patients with bipolar disorder have the right to know if lithium works for them.2
How Helpful is Lithium in Bipolar Disorder?
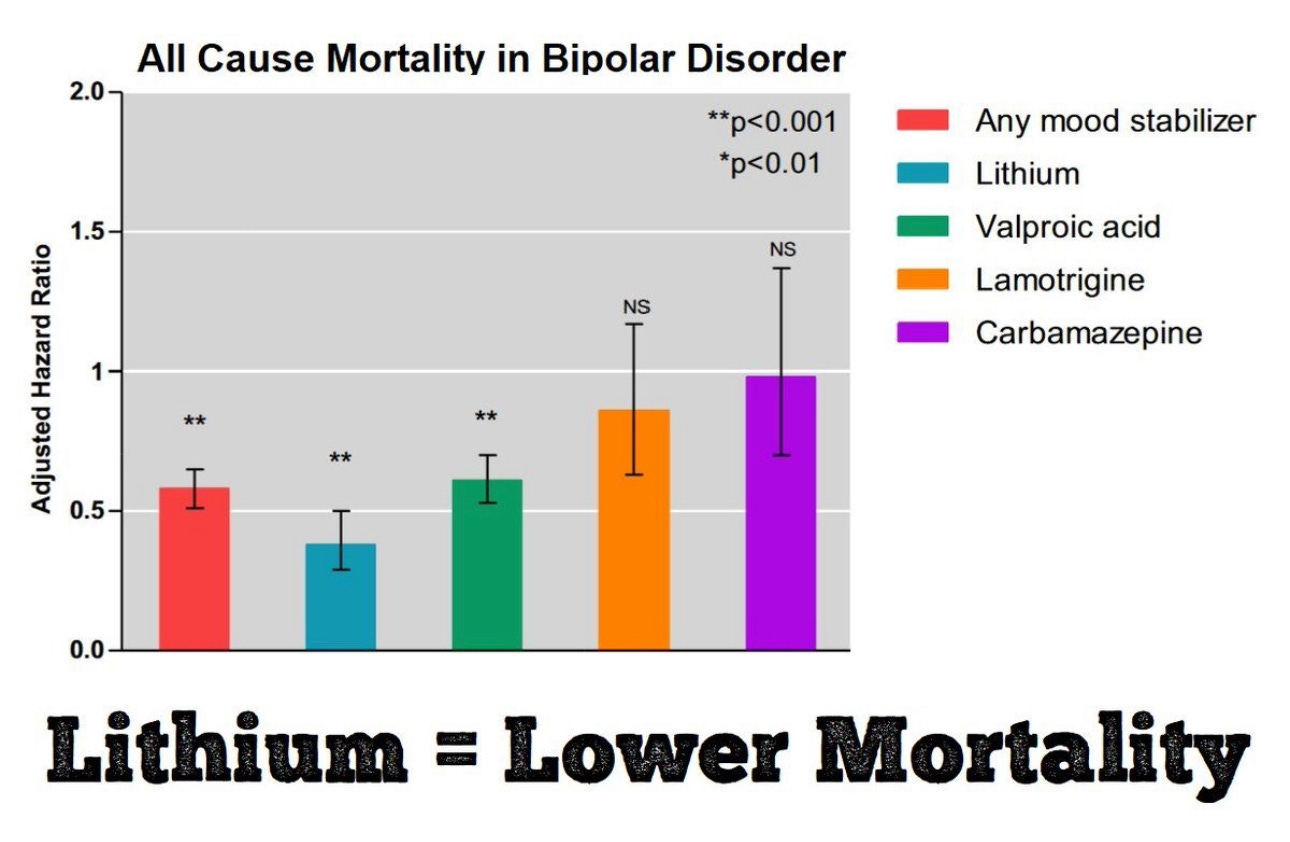
Lithium was associated with the lowest risks of all-cause mortality (aHR = 0.38, p < 0.001), suicide (aHR = 0.39, p < 0.001), and natural mortality (aHR = 0.37, p < 0.001).
Bipolar Disorder has, in most individuals, two different mood states that can be mixed and combined. When in an episode, people can experience symptoms of mania or depression, or mixed states with both. It’s an episodic condition by definition.
Bipolar disorder presents with periods of illness and periods of wellness. Unlike recurrent depression, where sufferers mostly just want it to go away, people with bipolar disorder often have a more nuanced relationship with their moods and cycles. Sometimes, they don't want to give up the mania. Lithium asks you to do so. And in exchange you get to live longer and be healthier. It's an existential bargain! If Mephistopheles were a psychiatrist, and Faust presented with bipolar disorder, the whole conversation would've been about lithium.
The data on bipolar disorder supports it as a modestly effective treatment for symptoms, mostly mania, beginning with its ability to treat acute—as in it's happening right now please make it stop—mania:
A network meta-analysis by Cipriani et al. found an effect size of 0.40 SMD [ed—Standard Mean Difference, in units of “Standard Deviations”], indicating a moderately sized effect, which is comparable to other anti-manic agents.
It’s not as sedating as antipsychotics, which makes it less appealing to inpatient psychiatrists who would prefer calm units. If it was a drug that made you taller, and you were a male human in America, it would add 1.2 inches to your height. The standard deviation is 3 inches, and the average height is 5’9”. To quote Skee-Lo: If you wished you were a little bit taller, lithium-effect size improvement would do it. If you wished you were a baller, this would not be a reasonable outcome to expect. For symptoms, it’s not a six-four Impala.
It is not an effective treatment for acute depression:
The available data strongly doubt the effectiveness of lithium in treating bipolar depression. The large EMBOLDEN I study found that lithium was not more effective than placebo in treating bipolar depression.
Very few oral medications are effective for bipolar depression. Bipolar depression has been historically very difficult to treat. But I believe that a narrow focus on symptomatology and episodic depression leads to getting the wrong answer in terms of a treatment goal.
The EMBOLDEN I trial above highlights the following findings:
Quetiapine (300 or 600 mg/d) was more effective than placebo for the treatment of episodes of acute depression in bipolar disorder. Lithium did not significantly differ from placebo on the main measures of efficacy. Both treatments were generally well tolerated.
Science is hard for episodic conditions with an ebb and flow. If bipolar depression “stayed still”, it would be easy to study. It doesn’t. It's very difficult to tell the difference between what would've happened naturally and what happened because we tried to intervene.3
If lithium isn’t a fantastic treatment for mania, and it isn’t a treatment for bipolar depression, why is this physician spending all this time writing about it? Because lithium prevents people suffering from bipolar disorder from death by suicide.
Psychiatry got it wrong. What if it’s not about treating symptoms? Lithium, by reducing death by suicide—without being great at treating depression—asks this crucial question. Lithium data says: treating symptoms is the wrong approach, it always has been, and it always will be, because people's lives aren't about symptoms. Plenty of people have symptoms of all sorts and don't kill themselves. Lithium is, in a way, an existential treatment. It's not an antidepressant, but you still won't kill yourself. We have extremely large data sets that demonstrate this is the case in unipolar or bipolar depression.
Suicide Prevention
The most important reason to consider lithium a first-line treatment is that people with bipolar disorder who take lithium are less likely to die by suicide. Let’s start by comparing people prescribed lithium… and compare adherence vs non-adherence:
The observed rates of suicide were 0.143, and of attempts, 2.01%/year, with a 5.2-fold (95% CI: 1.5–18.6) greater risk among patients consistently rated poorly versus highly adherent to lithium prophylaxis (11.4/2.2 acts/100 person-years).
Lithium, taken reliably, reduced the risk of suicide attempts by 500%+. Goodwin (of “Goodwin and Jamison” fame) peg that risk reduction even higher— 800% less likely to die by suicide. And given that 10-15% of people with bipolar disorder die by suicide, this is a huge deal. Kay Redfield Jamison writes compellingly about its effects in her many books, and notably, is a person with bipolar disorder who didn’t kill herself.
A large meta-analysis confirms this when compared to other treatments:
In these conditions, antidepressant treatment may not provide a beneficial effect on risk of suicidal thoughts and perhaps attempts, particularly in juveniles, whereas, lithium, perhaps even more than anticonvulsants, seems to be remarkably effective in preventing suicidal behavior. The mechanism of action is not well defined and may be associated with either a prevention of mood recurrences or a more specific “antisuicidal” activity.
This “better in youth” effect is notable because 50% of life-threatening suicidal acts in people with bipolar disorder happen in the first 7.5 years from diagnosis.
My Opinion:
Death-by-suicide numbers are grim—because of course, suicide is grim—but fewer completed suicides might mean less suffering before those avoided deaths also.
How Does the Body Process Lithium?
Lithium is a salt, and it’s cleared through the kidneys. It’s handled similarly to how sodium is dealt with—you pee it out. There is no “lithium receptor.” It has a lot of potential side effects (thanks to the Mayo Clinic for this guide!). There is no “metabolism” of lithium—it’s ingested and peed out, that is it. So the amount you consume, the amount of water you drink, and the rate at which you pee4 and sweat are what matters for the lithium level in your blood. And the level, as measured in the blood, matters!
A Curious History
Lithium was “discovered” as a modern treatment by accident. However, its initial applications were in the 19th Century, and John Cade was credited for its re-introduction to the field of Psychiatry in 1949.
The initial use of lithium was based on dosing given to rats. It appeared to calm them down. Human investigators couldn’t ask the rats why they looked calm… but it was probably because that much lithium makes any animal very sick to its stomach! Based on observation and its misinterpretation, it was given to humans in insane asylums and appeared to do something extraordinary for some of them. As a physician-scientist at Bellevue Hospital noted in 1871:
In 1871, William Hammond, professor of Diseases of the Mind and Nervous System at the Bellevue Hospital Medical College in New York, became the first physician to prescribe lithium for mania: “Latterly I have used the bromide of lithium in cases of acute mania, and have more reason to be satisfied with it than with any other medicine calculated to diminish the amount of blood in the cerebral vessels, and to calm any nervous excitement that may be present.”
When this made its way to the FDA, we get a sense of the poetry of the time that was perhaps more common then than we are allowed now:
At a meeting of the Psychopharmacologic Drugs Advisory Committee of the Food and Drug Administration (FDA) in the early 1970s, opinion was divided on using lithium for “the prevention of recurrent mania.” Gerald Klerman, professor of psychiatry at Harvard, was strongly in favor. But the FDA believed the indication ill-justified because of a lack of studies.
Klerman complained at another forum about the bureaucrats’ obduracy. He said he had objected to them that the literature wasn’t always perfect. “What about the first physician who used [lithium] and therefore couldn’t call upon a reasonably good body of evidence in the literature …?” he asked them.
John Jennings (from the FDA): “He’s like the man who ate the first oyster.”
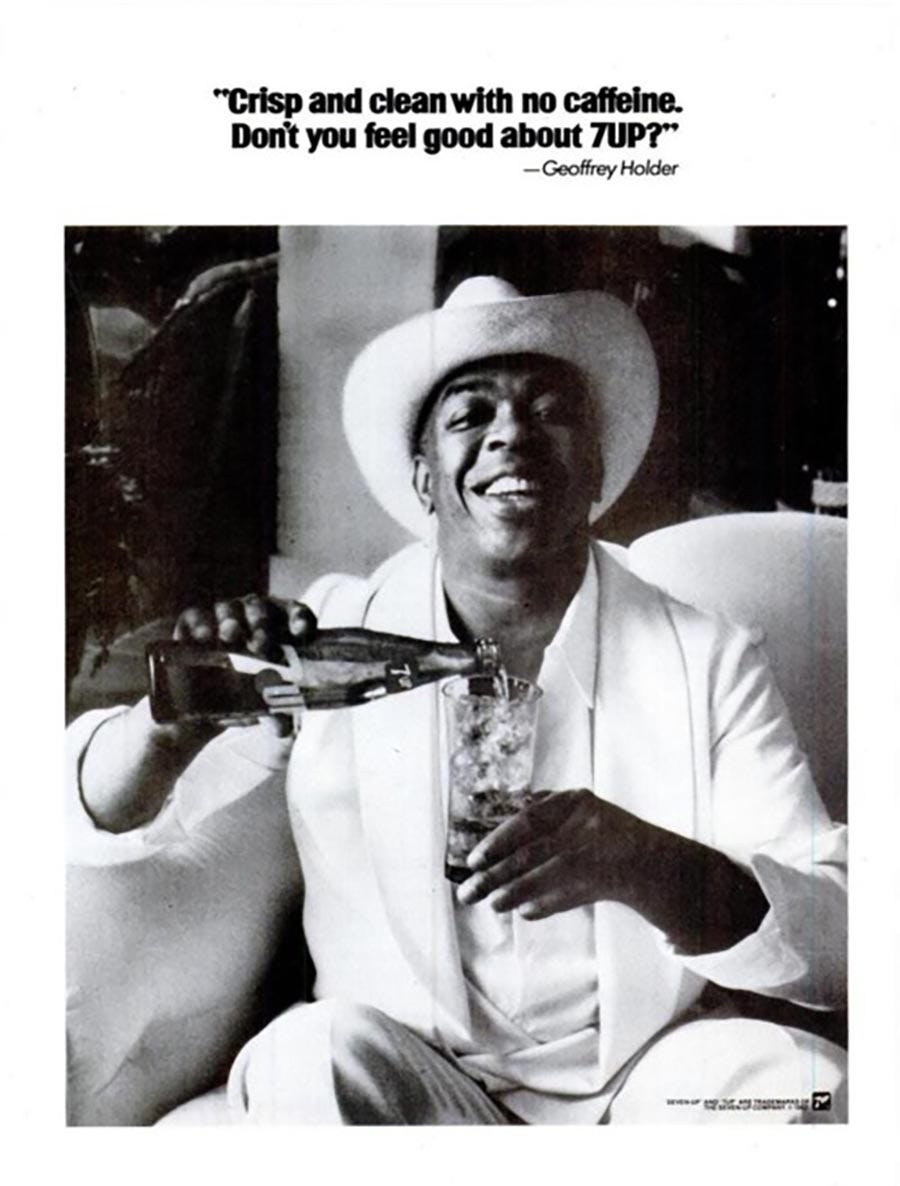
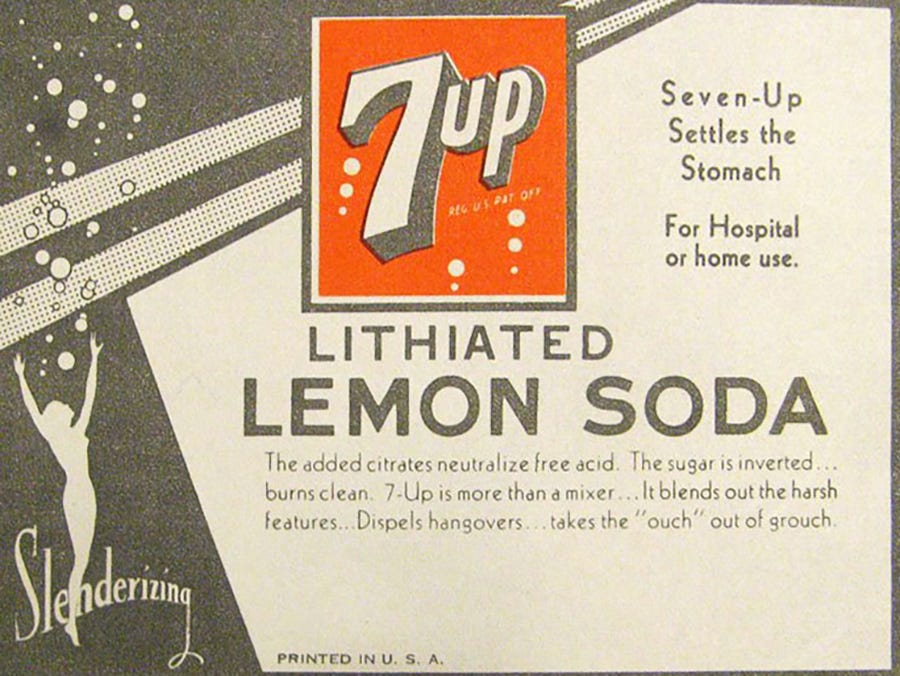
Something was UP with lithium!
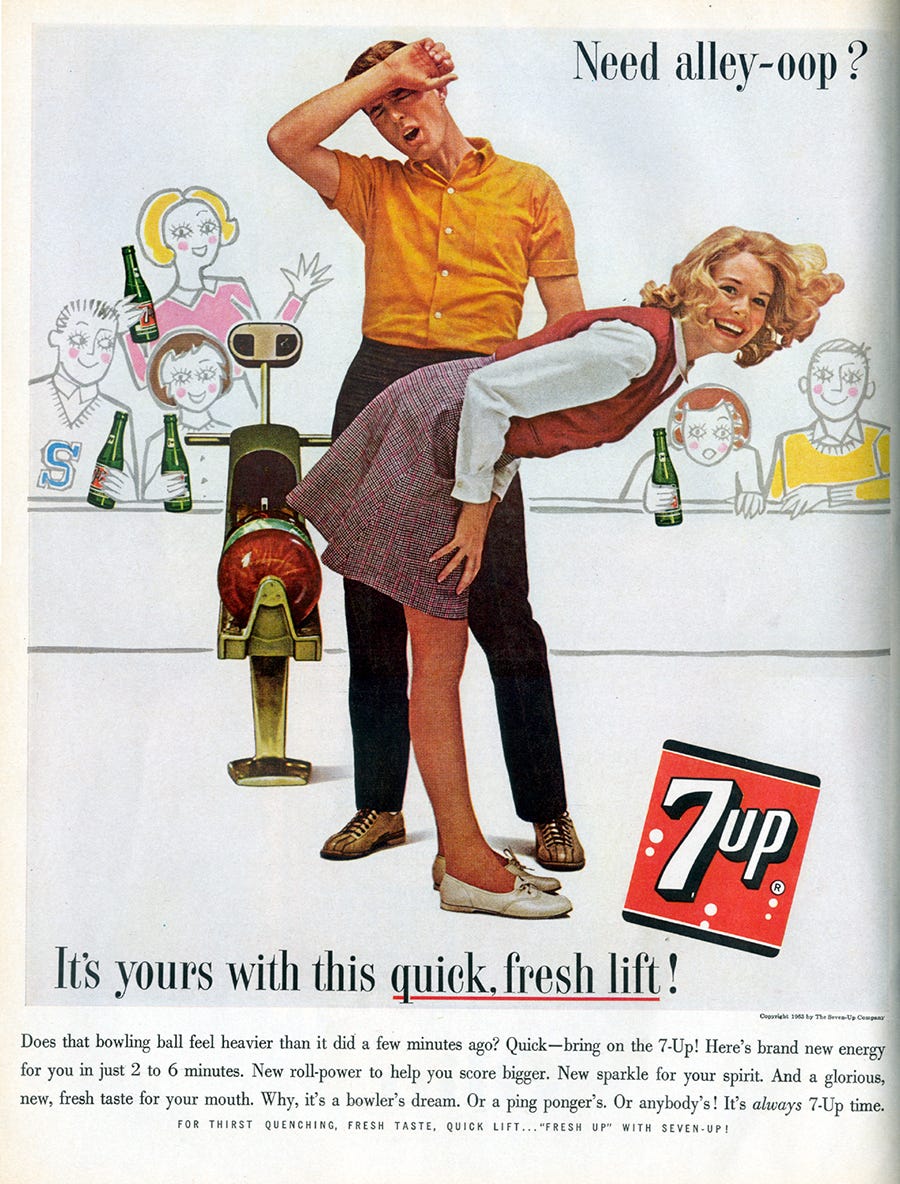
This is a joke, as lithium was an ingredient in 7-Up soda. Seven, in the title of 7-Up, is a cheeky reference to the atomic weight of lithium, which, as mentioned previously, includes three protons and four neutrons, thus having an atomic weight of seven. And it made you feel better, plausibly. Thus 7…and Up. It was originally created as a patent medicine, and acquired by Dr. Pepper, who apparently completed his residency in psychiatry. Thereafter it was acquired by Philip Morris. At some point, I presume, any mood-elevating compounds were eliminated to privilege the primary profit-making compound in the Phillip Morris portfolio, which is overwhelmingly nicotine, and secondarily fructose.
Yes, that is right. The lemon flavor of 7-Up is there to add Citrate… thus the solubility of the lithium citrate…which is still a format for lithium medicine to this day.
What Forms of Lithium Exist?
Basic lithium without any “extended-release” anything is available as a tablet in the form of lithium carbonate.
In liquid form, it’s lithium citrate.
In extended-release versions, the tablets are available as riffs on “lithiobid”…aka twice-a-day lithium: Lith…o…B.I.D.
It is an abbreviation for "bis in die" which in Latin means twice a day. The abbreviation b.i.d. is sometimes written without a period either in lower-case letters as "bid" or in capital letters as "BID".
It’s other extended release version is called Eskalith CR, for Controlled Release. From the much less poetic package insert for this medicine:
ESKALITH CR Controlled-Release Tablets: Each round, yellow, biconvex tablet, debossed with SKF and J10 on one side and scored on the other side, contains lithium carbonate, 450 mg. Inactive ingredients consist of alginic acid, gelatin, iron oxide, magnesium stearate, and sodium starch glycolate.
The crucial takeaways:
Lithium Carbonate comes in 300mg tablets.
Lithium Citrate is a liquid—you aren’t limited to the pill to determine dose.
Lithobid ER comes in 300mg tablets.
Eskalith CR comes in 450mg tablets.
And—among the most crucial details in psychiatry—you can break Eskalith in half and not destroy its time-release mechanism. This is true with almost nothing else. Crushing it destroys the extended release-ness, but cutting it in half doesn’t.
My Opinion:
In the most personal of opinions, the above pill sizes are a disaster. Almost no one takes one lithium pill as their dose. Thus, the fact that everyone taking lithium is taking some pills and maybe breaking them in half sucks. It makes you feel stigmatized, and it’s harder to remember. There is a physical limit around how big a pill can be when it contains an inorganic salt, but the experience of people taking medicine was ignored. More pills feel weird. It’s easy to screw up. So, in case Mark Cuban’s Cost Plus Drugs team is reading, I’d love to see the following:
Dr. M’s Lith-o-sure: A new formulation of lithium that is basically Eskalith CR but comes in: 600mg, 750mg, 900mg, 1100mg, 1200mg, 1350mg, and 1400mg.
Or whatever the limit is on the size of the pill. It will not be a money maker, but it will be important.
How Should We Dose Lithium?
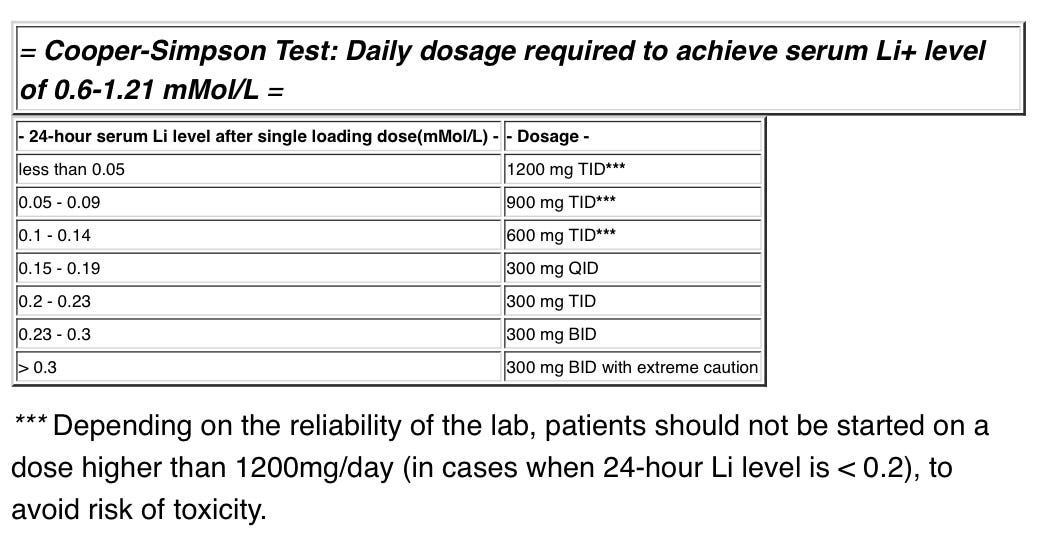
I strongly advocate starting with the Cooper-Simpson method when determining lithium dosage.
The idea, from work back in 1974:
A test dose of lithium (600mg of Lithium Carbonate) is given, and
A blood level is drawn 24h later. Then, it’s compared to the table below.
We only get one shot at this test—because it’s only validated for the first time you ever take lithium.
The traditional way—before 1974, but still widely used—of dosing lithium…sucks. Start with a low dose, given its 5-day half-life, and then you must get blood drawn every five days to determine the dose adjustment. Thus it takes weeks and weeks and blood draw after blood draw.
The blood level we are aiming to achieve is still a matter of some debate:
The efficacy of lithium is dose-dependent and reliably correlates with serum concentrations. It is now generally accepted that attention should be maintained between 0.6 and 0.8 mmol/L, although some authors still favour 0.8-1.2 mmol/L.
Higher blood levels are recommended in extended-release formulations of the drug.
The close-to-canonical Carlat Report has this interview with editor Chris Aiken, M.D. where he explains:
Chris Aiken, MD: Lithium is often dosed twice a day, but I think that's out of convention rather than science. Its half-life is 24 hours, so there's no reason to do that. And in a few long-term studies, patients had lower rates of renal problems if the lithium was dosed entirely at night rather than twice a day. The kidneys seem better when they get a bolus of lithium at night rather than spread evenly throughout the day.
Most people take between 900mg and 1350mg of lithium daily as a bipolar disorder treatment, which is limited by tolerability.
My Opinion:
Dosing should be LITHIUM ALL AT ONCE, AT NIGHT. It’s safer and, importantly, vastly more likely to be taken reliably.5
The starting dosage can be determined by the Cooper-Simpson method. Start at the dosage recommended by the test dose. Then get a lithium blood level drawn five days later. This will be a steady state blood level. As a basic guideline, adjust medication dosage to get to a 0.8 blood level. There is evidence that lower blood levels aren’t as helpful, such as the LiTMUS trial found with low-dose lithium augmentation:
Results: The authors observed no statistically significant advantage of lithium plus [Oral Current Meds that Weren’t Lithium] on CGI-BP-S scores, necessary clinical adjustments, or proportion with sustained remission. Both groups had similar outcomes across secondary clinical and functional measures.
And when half of the patients with bipolar disorder stop their treatment, we have a long way to go, which we must take seriously in a regularly devastating illness that doesn’t have to be.
A note on lithium blood level interpretation: All of the published levels for lithium dosing are based on twice daily dosing, and are by definition trough levels, drawn 12 hours after the dose from the evening before, but before the morning dose. Practically, this means that any blood level drawn after once daily dosing all at night is going to be different than what it would’ve looked like—on the high side—for twice daily dosing. This is one of the reasons that start with the Cooper-Simpson method. It’s also a reason that a blood level drawn in the emergency room is almost completely meaningless, unless it happens to be dangerously high, or by chance, drawing 12 hours after the PM dose a person had. Almost axiomatically, patients are rarely showing up in the ER at 9 AM when in crisis with bipolar disorder, because that’s just not when people tend to show up in crisis, particular if they took their dose the night before precisely 12 hours earlier. If you want to be extremely accurate with your lithium level understandings, and have a very compliant patients, you can have the individual split their dose into a.m. and p.m. doses for the five days prior to the lithium blood draw, and then get a true trough dose that will be in keeping with everything you’ve ever read. This approach is clumsy, and so what I usually do is draw one blood level like this, and then another blood level with the “all at night” real world dosing, and then compare the two so I know what the rough equivalent is for that person. Then all of my future blood draws can be calibrated against those two initial assessments.
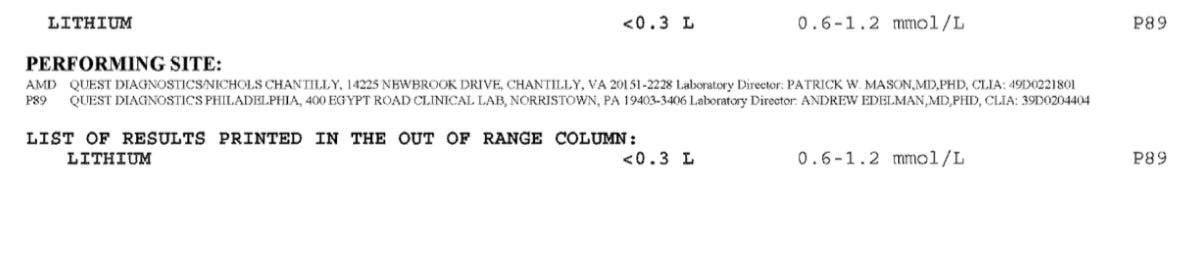
When I did this with my patient this week, thanks to my EHR’s Quest integration, I got back the following unhelpful result:
I had to call Quest and make a request for this lab and all future labs to have different reporting parameters—because “<0.3” is completely useless for the Cooper-Simpson test. But it’s better than most every other mental health EHR product that has zero lab integrations whatsoever for small psychiatry practices.
And Now For The Most Commercially Biased Opinion and Disclosure of this Article:
No one has to remind you to check your text messages or other notifications on your phone. We know how to shape behavior. I think the better future of healthcare includes “adherence augmentation” with technologies like iRxReminder (a company at which I’m now Chief Medical Officer).6
Lithium in Pediatric Bipolar Disorder
Pediatric bipolar disorder has taken a real beating as a diagnostic entity recently. When the Mayo Clinic uses click-bait tiles like “Bipolar Disorder In Children: Is it Possible?” we know there is a real problem.
(Short Answer: Yes. Yes, it is. I also lived it. H/t to Manpreet Singh, M.D., M.S. for her advocacy on the topic).
Cutting to the chase: Lithium is a better treatment for young people with bipolar disorder than antipsychotic medication or other “mood stabilizers”:
Available evidence suggested that in early illness course, lithium use was associated with lower recurrence risk compared with other mood stabilizers [Ed: e.g., Depakote, tegretol]. Mood stabilizers [Ed: Including lithium] were also associated with better global functioning, compared with antipsychotics in the medium term.
It’s worth noting that in youth, lithium treatment has been proven effective in RCTs for youth both with “just” bipolar disorder and with bipolar disorder with co-occurring substance use disorders.
My Opinion:
Lithium is safer and more effective than any other medicine (on average) for kids with accurately and carefully diagnosed bipolar disorder and should be offered first.
The Side Effects are Complicated and Variable
Almost everyone gets more thirsty and has to pee more. In medicine speak, this is called polydipsia and polyuria. It’s salt tablets. Of course, you will drink and thus pee more.
Death by Overdose: The most serious risk is lithium toxicity and eventual death. Don’t overdose on lithium. It’s very bad. Don’t get wildly dehydrated. Also bad. This starts as nausea, and progresses to confusion, delirium, and worse. The lethal dose is on the order of 15 days of medicine for most people, at around 100mg/Kg for and LD-50 (this defines the legal dose for half of people). It's rare that this would happen by accident.
Lithium Toxicity: Lithium at concentrations above 2 mMol/L leads to a constellation of symptoms:
Lithium toxicity can cause interstitial nephritis, arrhythmia, sick sinus syndrome, hypotension, T-wave abnormalities, and bradycardia. Rarely, toxicity can cause pseudotumor cerebri and seizures. Lithium toxicity has no antidote. Treatment for lithium toxicity is primarily hydration and to stop the drug. Give hydration with normal saline, which will also enhance lithium excretion. Avoid all diuretics. If the patient has severe renal dysfunction or failure, or severely altered mental status, then start with hemodialysis. 20 to 30 mg of propranolol given 2 to 3 times per day may help reduce tremors.
My translation into everyday language: It causes problems with your heart— beating too slowly, or out of sync—confusion, nausea, vomiting, you will feel very, very sick and then totally “out of it.” Hydration and in extreme cases, dialysis is required. Avoid this situation! It’s a horrible way to feel and a horrible way to die—see “don’t overdose on your lithium” as a suicide attempt methodology above.
Kidney Injury and Chronic Kidney Disease: Long-term treatment with bipolar disorder needs to be monitored for safety because injury to the kidneys happens in patients with bipolar disorder, both looking at kidney function in a lab test and clinically:
Among 154 patients who received [Long term lithium therapy] , 41 patients (27%) developed CKD, of whom 20 (49%) patients continued lithium (continuers) and 19 (46%) discontinued it (discontinuers). The median time to stage 3 CKD development was 21.7 years from the start of Li treatment.
However, diabetes and chronic kidney disease go together, and it is not conclusive that “lithium did it” all on its own.
There was no significant difference in the progression of CKD among Li continuers versus discontinuers, at the mean follow-up duration of 4.2 years, after the CKD diagnosis. Progression of CKD could be influenced by existing comorbidities and may not necessarily be due to lithium alone.
My Opinion:
Monitor kidney function. Metabolic health is more important after 20-30 years in most people, and we owe it to our patients to help preserve their health, not just their mental health. Practically, reducing the risk of weight gain needs to be a focus of psychiatric care.
The most important way to reduce the risk of kidney damage is to tell any health professional that you are taking lithium and avoid NSAIDS for pain other than Sulindac, a safe pain medicine for individuals taking lithium. NSAIDS include medications like Advil and Aleve.7
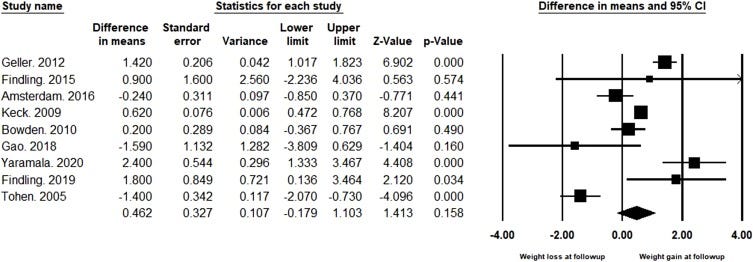
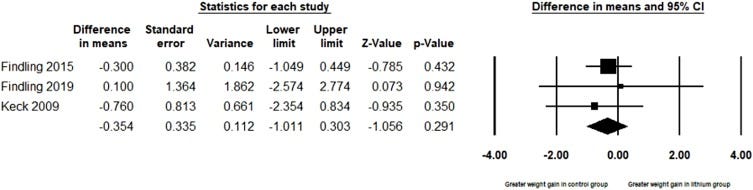
Weight Change: Although it’s clear that many medications have weight gain as a side effect, the most up-to-date meta-analysis of 991 patients tells a more hopeful story about lithium metabolic consequences.
The headline is: Lithium doesn’t cause statistically significant weight gain.
The difference in weight between lithium-treated patients at follow up compared to baseline did not reach statistical significance, reporting weight gain of 0.462 Kg in the lithium group (Difference in means = 0.462, 95 % C.I.= -0.179 to 1.103, p = 0.158, n= 991). Heterogeneity for this outcome was high (I2 = 89 %).
The above graph, for general audiences, has that little diamond at the bottom. When those cross zero (the line in the middle) it means that there is no difference, from a statistical perspective.
When only comparing lithium to placebo, the trend was towards weight loss, but again the diamond at the bottom crossing zero means no significant difference:
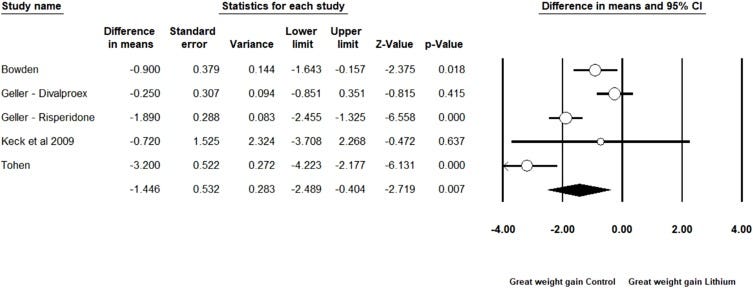
And the most important finding, to me, is that lithium is significantly safer than other options when it comes to weight gain:
Cognitive Impairment: I don’t have a great answer. The shortest answer: cognitive impairment—this is real, but happens anyway, in a progressive illness like bipolar disorder:
Conclusion: Patients with bipolar I disorder have verbal memory deficits that are not explained by medication or by lithium monotherapy, but by the condition itself.
Hypothyroidism: It happens, it’s a real adverse effect. It’s treatable:
The prevalence of clinical hypothyroidism was increased in patients taking lithium compared with those given placebo (odds ratio [OR] 5·78, 95% CI 2·00–16·67; p=0·001)
500% higher risk than placebo, but also relatively rare.
Tremor: It’s real. It happens:
Lithium tremor is classified as a postural tremor and subcategorized as an exaggerated physiologic tremor. Differential diagnosis includes metabolic abnormalities, benign essential tremor, Parkinson's disease, and lithium toxicity.
The tremor is dose-dependent and needs to be differentiated from other causes of tremor. It won’t stop you from being a surgeon either, cause propranolol works to mitigate the problem. At the end of the day, tremor from lithium is an exaggeration of physiological tremor, and it gets worse with higher dosages. This is a big deal and patients who use their hands for work or play and need them to be steady. Photographers, surgeons, and artists are all special populations. Tremor can be embarrassing in public. Soup, for example, is an issue. Soup spoons are an issue when too shallow. The side effect is completely dose-dependent. It was easier to evaluate this when all psychiatry was in person, but when it comes to tele-health, we're gonna need to do a better job of collecting this data.
Blood Disorders: Lithium is a complex molecule when it comes to the blood, and causes a number of abnormalities on white blood cell testing (“Complete Blood Count” or CBC in lab-speak). That having been said, many of these changes are in what is tested—you see more white cells moving into the testable blood from the peripherally of blood vessels where they usually hang out. These changes can be reviewed in fine publications like this one. Other rare side effects include: bleeding and fatigue, suggesting the need for another complete blood count.
Diarrhea and Nausea: These side effects are common (10-20% of people) and peak blood level related. They also get better with time.
Severe Acne: More common than I thought… up to 45% of people taking lithium will have some skin problem. Dermatology can fix most of these problems—Accutane exists, and its causal role in risk for suicide has not been supported by a detailed reviews of the evidence:
A causal relationship between isotretinioin and psychiatric morbidity, including depression and suicide, has not been demonstrated. In fact, there is evidence that acne itself is associated with psychiatric morbidity and that isotretinoin may attenuate the effect of acne on this psychiatric morbidity.
Birth Defects in Pregnancy: There is a 2.14% risk of Ebstein’s Anomaly, a correctable heart defect, in children exposed to lithium in utero. Perinatal psychiatrists specialize in these sort of questions8. I’m looking at you, The Motherhood Center. Before anyone goes off the deep end about this, 100% of the people I've ever met with bipolar disorder are the children of people who had the genetics for it. It doesn't mean you can't have kids. It doesn't mean you can't get pregnant. It doesn't mean you'll be a bad parent. You can absolutely, positively, have children and have bipolar disorder and have it be fine. Please don't make decisions for your future children and their existence, or lack thereof, based on your fears of being a broken person because of bipolar disorder or lithium treatment.
Erectile Dysfunction: It happens. It’s relatively common (25-30% of patients will report some sexual function problem if asked). The pathophysiology is complex:
Stendra also exists and works quite a bit faster than viagra (30m as opposed to 2h for the drug to start working). These are reasonable options if this side effect presents itself. Expect to fight for prior authorization. Feel free to send them this article for the auth.9
Suggested Monitoring Schedule:
Monitoring should be done every 1 to 2 weeks until reaching the desired therapeutic levels. Cooper-Simpson test to accelerate the time-to-therapeutic dose, and thus reduce the time it takes for patients to feel well.
Then, check lithium levels every 2 to 3 months. It is also important to monitor patients for dehydration and lower the dose when there are signs of infection, excessive sweating, or diarrhea. Toxic levels are when the drug level is more than 2 mEq/L.
Lithium: It’s Remarkable. And Can Be Pretty Mellow…
As this guitar-harp cover makes clear, in musical format:
Lithium presents us with a quandary. It doesn't treat depression in bipolar disorder. But people don't kill themselves and don't die for other reasons at vastly lower rates. This begs the question: if treating depression isn't the mechanism by which people don't die by suicide, what the hell is happening?
The answer is: We don't know. Death by suicide and depression have a relationship. Being sad and killing oneself seem obviously connected—except that for some people, a treatment that doesn't impact acute sadness and depression effectively is better than effective antidepressants. I don't think this is accidental. I think there's a fundamental problem with our understanding of suicide as a consequence of a depressed mood.
Now that I've called into question everything you understood to be true, I'm going to thank you for reading and encourage you to share this and subscribe.
In Summary, for people considering lithium themselves as a treatment option:
Lithium works for bipolar disorder, but not for everyone.
When it works, it saves lives.
It doesn’t typically cause weight gain.
There are lots of side effects that are possible, but they are mostly dose-dependent—if you're choosing a treatment option based on what the side effects might be, you're missing out.
Close monitoring is essential.
Drink plenty of fluids
No Advil, Naproxen, or most NSAIDS—ask about Sulindac!
For Prescribing Doctors, NPs, and PAs:
Lithium is a first-line treatment for bipolar disorder.
Understand the risks, and listen to your patient’s experiences closely! Most side effects are possible with lithium.
Cooper-Simpson Test Dose/24h level gets lithium started quicker!
Monitor blood levels, kidney and thyroid function every 3 months, and if this is not easy for you, get technology to help you (My EHR integrates with Quest, LabCorp, and even at-home blood testing companies).
Offer lithium at every visit till someone is willing to give it a shot—you don't have to be pushy about it, but expect patients to say no, and accept the answer. With each relapse that could've been prevented by lithium, remind your patients that lithium is a great option for longer, healthier lives in bipolar disorder.
Your patients have a right to know if they are lithium responsive, and they have a right to not take that treatment if it's not tolerable.
It’s worth noting Radiolab creator Jad Abumrad stepped away from this remarkable show in 2022, leaving it in the capable hands of Lulu Miller. It’s a significant change and an important one. It’s also worth noting this show changed podcasts and science journalism forever. We owe them a debt.
Even if you’re not going to take lithium all the time, it’s still worth knowing if it helps you. When I’m explaining lithium as an option for patients, I’m generally introducing it as a trial of a medicine to see if it’s something we want to have in the back pocket should we need it. Some people continue to take medication, and some don’t find it terrible, but it’s worth knowing if it works for you.
This inability to tell the difference because of underlying variability is the core of why bipolar disorder is complicated to study or treat.
Once Daily (OD) dosing of all medicines vastly outperforms multiple times a day dosing (at the meta-analysis level):
OD schedules were associated with higher adherence rates (odds ratio [OR] 3.07, 95% confidence interval [CI] 1.80–5.23; P < 0.001 for OD versus > OD dosing)
Lithium: a 300% better medicine if dosed once daily.
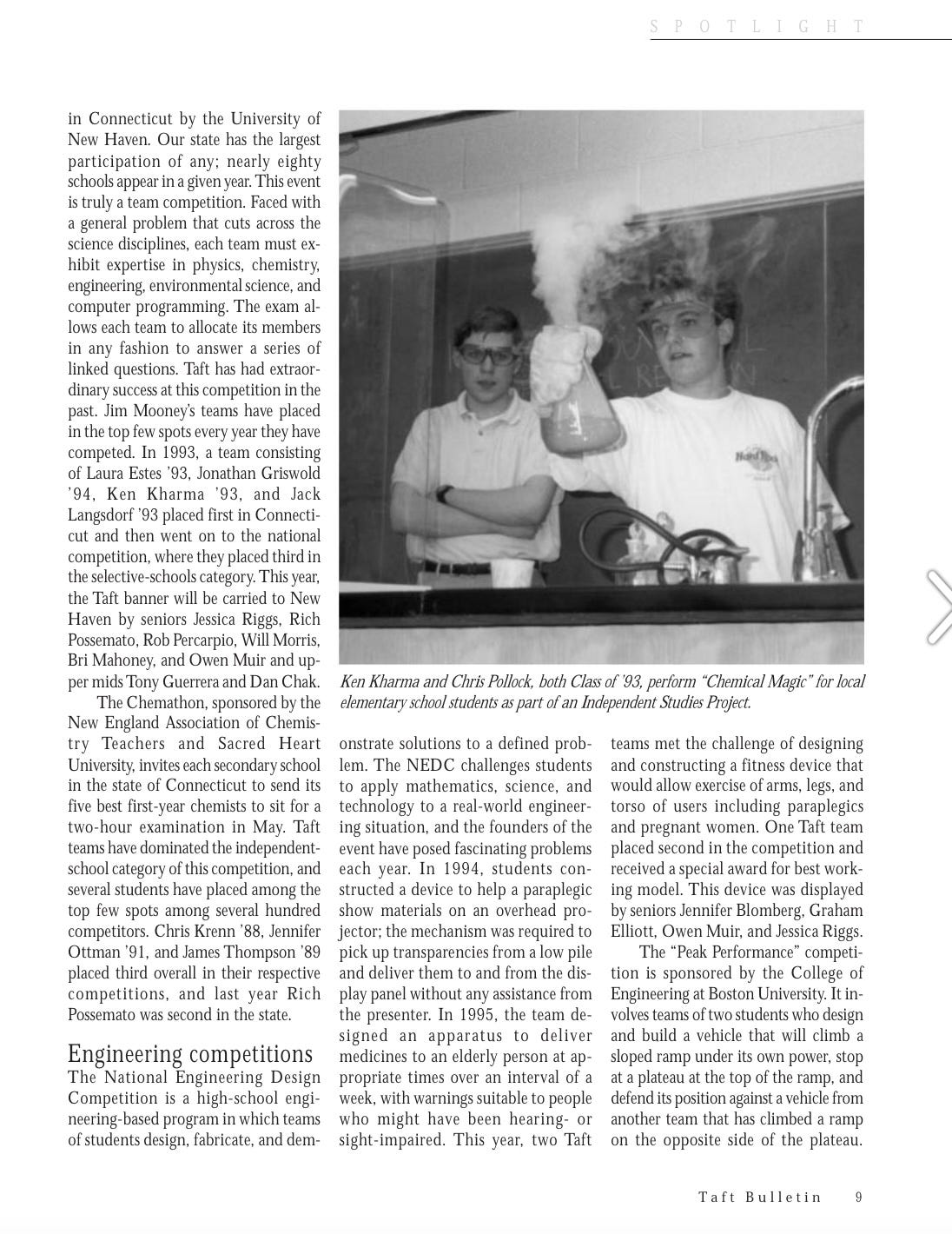
Technology-enabled medication adherence is a problem I've been grinding away at since 1995. Yes, that is when I won a prize in the national engineering design challenge with my team at the Taft School, from which I graduated in 1997… for an automated pill dispensing technology. Given some of our alums, this was not a slouch cohort.
I’m like a dog with a bone some times. We won best working model in ‘95, but not 1st Place.
This gets into some renal physiology here, but NSAIDS act on both COX 1 and COX 2, expressed in the kidneys:
COX-1 functions mainly in the control of renal hemodynamics and glomerular filtration rate (GFR), while COX-2 functions primarily affect salt and water excretion. Blockade of either or both of these enzymes can have, therefore, different effects on renal function.
And meds like naproxen and ibuprofen both act on COX1 + COX2, reducing GFR ( so less filtering in the kidneys = less lithium clearance).
Recent large studies have confirmed the association between first-trimester lithium exposure and an increased risk of congenital malformations. Importantly, the risk estimates from these studies are lower than previously reported. Tapering of lithium during the first trimester could be considered, but should be weighed against the risks of relapse. There seems to be no association between lithium use and pregnancy or delivery-related outcomes, but more research is needed to be more conclusive. When lithium is prescribed during pregnancy, lithium blood levels should be monitored more frequently than outside of pregnancy and preferably weekly in the third trimester. We recommend a high-resolution ultrasound with fetal anomaly scan at 20 weeks.
If anyone actually does send this article as part of a prior authorization request, please let me know, I will be so happy.





"If it was a drug that made you taller, and you were a male human in America, it would add 1.2 inches to your height. The standard deviation is 3 inches, and the average height is 5’9”. To quote Skee-Lo: If you wished you were a little bit taller, lithium-effect size improvement would do it. If you wished you were a baller, this would not be a reasonable outcome to expect. For symptoms, it’s not a six-four Impala."
That's... that's potentially the greatest explanation of anything I've ever heard.
This is fantastic!