The Frontier Psychiatrists is a daily-enough health health-themed publication. Today, I’m reviewing the data on GLP-1 drugs (short for Glucagon-like Peptide-1) as they apply to substance use disorders. I’ve written about my journey with weight loss and DM II, which, thanks to these drugs, I no longer have.
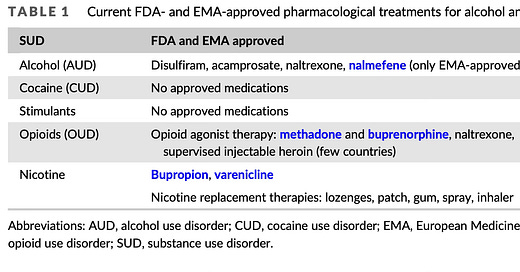
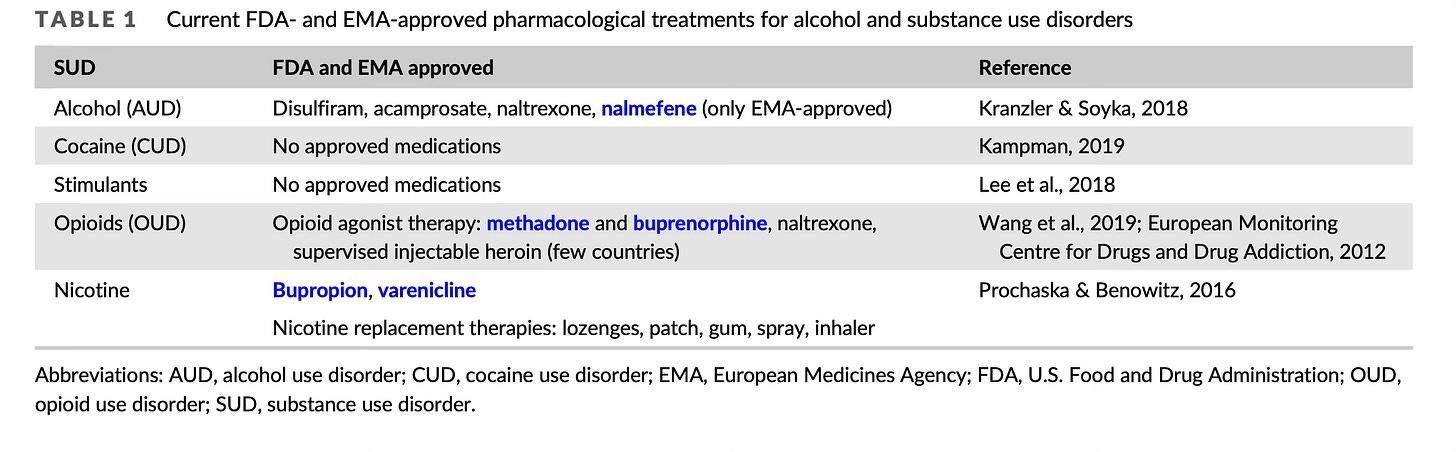
To set the stage, addiction sucks. We also have limited treatments available to relieve the suffering of addictive disorders. Here is a chart1:
We don't have that much. We have no biological treatments approved for the treatment of cocaine or stimulant use disorders. We have a few studies on transcranial magnetic stimulation23, one of which I wrote 4!
Reward circuitry is hard to overcome because it's crucial to our existence. I've written before about the role of the nucleus accumbens (NAc), a structure deep in the brain where dopamine binds to receptors that give us the sense of feeling good. Without the NAc, we wouldn't have goal-directed behavior, and we would all die. Nothing would be worth it. Dopamine release in this small structure deep in the brain is what we mean by “worth it.”
Thus, we can understand that biological treatments intervening in this crucial structure will have a hard time getting it to accomplish anything other than what it's biologically attuned to. The problem with addictive drugs is that they jack into this reward system and have an extremely hard time being pried out.
Addictions are sticky because staying alive is sticky, and feeling good is sticky because of course it is. We do have a recent example of a series of compounds that altered the underlying biology in the direction of health. That's glucagon-like peptide 1 drugs. This includes Semeglutide (aka Ozempic and Wegovy) and related compounds.
These medications address satiety signals in the brain—the sense of having had “enough” which extra-sugar does a good job of breaking. A nice review in BMJ5 recently addressed the evidence, which is mostly pre-clinical (we've done science in animals, and we have trials enrolling in humans, but we don't have evidence from those trials published yet). Here are some of the proposed mechanisms: