fMRI Guided Accelerated TMS for Bipolar Disorder...Maybe
Yet another Ode to Table One from Dr. Owen Muir.
As a newsletter author with bipolar disorder who happens to be a psychiatrist who deploys accelerated transcranial magnetic stimulation, it is a bit strange for me to be offering the following article taking issue with published research on the condition I have, with positive findings. Still, it's 2024, so I guess this is…just what's happening?
I've written about bipolar on numerous prior occasions and was treated with transcranial magnetic stimulation over a decade ago. I have a dog in this fight.
A paper was recently published in JAMA Psychiatry, demonstrating aiTBS (accelerated intermittent theta burst stimulation—a pattern of brain stimulation using transcranial magnetic stimulation (TMS) devices) in the treatment of “treatment-refractory bipolar depression.”
Readers are wondering: does the title accurately describe the paper? That title:
Accelerated Intermittent Theta-Burst Stimulation and Treatment-Refractory Bipolar Depression: A Randomized Clinical Trial
My argument? A careful reading of this clinical trial will demonstrate not all is as it seems…
Before we dig into this paper, we must illuminate some things that might not be common knowledge. Bipolar disorder is known to have variants. Some details in those variants. Thanks to the machinations of Abbott pharmaceuticals, manic depressive illness, a serious problem that required serious medications like lithium, was reclassified as bipolar disorder to help sell Depakote.
Look, I know that's a broad statement, but it is true enough. I'm sure the people who made those changes thought it would be useful-ish and sciency. Still, Psychiatrists have been easy to seduce by Pharma for a long time. To imagine that this group of psychiatrists was somehow immune to the machinations of billions of dollars in market cap stretches my credulity. If I'm wrong, and you were there, please feel free to write me.
Not only did we get one bipolar disorder, we got two. Instead of understanding bipolar disorder to have a unitary nature with different levels of severity? We made a different diagnosis, which we called bipolar II, and decades of misdiagnosis ensued.
Bipolar II might exist. I'm not saying it doesn't exist as it is defined. I'm just saying it's unhelpful. The concept was that there exists a cohort of people with bipolar disorder who never get “full-blown” mania and only ever get mild mania (“hypomania”) but still have bipolar depression as their version of depression. This, to the best of our knowledge, is a rare phenomenon:
The aggregate lifetime prevalence of Bipolar-I disorder was 0.6%, Bipolar-II was 0.4%, …Twelve-month prevalence of Bipolar-I disorder was 0.4%, Bipolar-II was 0.3%1
Setting aside my nagging “Does bipolar II as a concept add anything?” argument, with regards to the science questions regarding bipolar disorder, the best data we have indicates that Bipolar II is more rare than Bipolar I disorder by a factor of “a bit.”—it is about 1.5:1. We have the additional detail, as I have discussed previosuly, that oral antidepressants don’t work in bipolar disorder:
Among 5 001 treatment studies published, 14 double-blind randomized controlled trials involving 1 244 patients were included in the meta-analysis. … Studies suggested that patients treated with antidepressants were not significantly more likely to achieve higher response and remission rates in the short-term or long-term treatment than patients treated with placebo and other medications. Antidepressants were not associated with an increased risk of discontinuation, relapse or suicidality. When one antidepressant was compared with another, no significant difference in efficacy and tolerability was found.2
“Antidepressants” are not effective medicines for bipolar depression.
With all that information in hand, let’s look at the aiTBS for bipolar depression study. The first question I am asking is also the most problematic…who is in the sample? The inclusion criteria were:
Participants were recruited from March 2022 through February 2024. Inclusion criteria included a primary diagnosis of BD depressed phase, an MADRS score of 20 or higher,5 age 22 to 70 years, receipt of 2 or more failed treatments by Antidepressant Treatment History Form criteria,6 and initiation of a stable mood stabilizer regimen 4 or more weeks prior to aiTBS.3
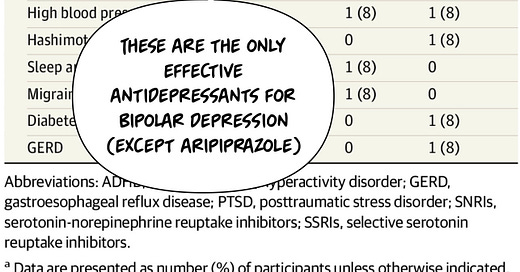
Next, we will look at…come one, it’s The Frontier Psychiatrists! It’s table one! We love table one around here! A somewhat perplexing thing I will point out is that the medications patients in this theoretically bipolar disorder study were historically taking were only occasionally effective treatments for bipolar depression:
There are a lot of reasons that patients with bipolar disorder might have been prescribed medications that don't treat bipolar depression. This has been an issue for years in the field of psychiatry, where people either don't make the diagnosis of bipolar disorder or don't understand what treats it. To be clear, anti-depressant medication does not treat bipolar depression. They don't work. I've already said that before; many papers establish it, but that's one of the many reasons that I think this is a “suss” sample—my kids are 8, and I’m on TikTok.
People have known those medications don't work and bipolar depression for quite some time. Over a decade, in fact. So why are we still looking at ineffective medications in a study on bipolar depression? Why are we using the anti-depressant treatment history form? The ATHF is an inappropriate tool in a study for bipolar depression. It's a tool evaluating treatments that don't work for a condition people don't have. It would be like evaluating antibiotic resistance in a study of a virus. It's just an inappropriate measure. Unless, of course, you suspect the sample of theoretically bipolar disorder having depressed individuals don't actually have bipolar depression. What if you think they might have unipolar depression?
It's pretty easy to have depression when you have unipolar depression, as long as you're talking about prior episodes, and you're presenting as very depressed, and none of your prior episodes were frankly manic. Let's dig back into Table One to see the ratio of bipolar two to bipolar one in this sample.
Oh my, that ratio of vastly, overwhelmingly bipolar two patients compared to bipolar one patients is exactly the opposite of what we would expect in the community by chance and then skewed a little bit further in the wrong direction.
So either the recruitment for the trial had something extraordinary and statistically unlikely to occur, which is that greater than 90% of the patients walking in the door for a bipolar disorder study had a rare type of disorder, or…it's a lot of people with depression who wanted to get into an accelerated TMS study. Keep in mind — the out-of-pocket cost of this treatment is still currently on the order of $36,000 for a course of treatment for depression. And yet we wonder, did research subjects have any incentive to misrepresent their condition to researchers? If I were inclined to misrepresent my condition to researchers to get treatment for free, it's just a lot more plausible to say you have bipolar II—currently depressed—and felt manic that one time.
At the bare minimum, this study should be titled “Accelerated Intermittent Theta-Burst Stimulation and Treatment-Refractory Overwhelmingly Bipolar II Depression: A Randomized Clinical Trial.”
It might even be a touch more honest to have titled it something like “Accelerated Intermittent Theta-Burst Stimulation in a mixed sample of both Treatment-Refractory Bipolar Depression and unipolar depression among those who Felt Compelled to Represent their Depression as Dipolar in order to be Randomized to get a Very Expensive fMRI- guided Neuromodulation technique to treat their Depression: A Randomized Clinical Trial.”
Regardless, in the population who may or may not have had bipolar disorder, the treatment worked:
I'm not saying this is not an effective treatment; I am saying I'm not convinced this sample actually has bipolar disorder. Also, people are credulous. That, I will believe any day.
Zhang, Yingli1,2,; Yang, Huan1; Yang, Shichang3; Liang, Wei4; Dai, Ping5; Wang, Changhong2; Zhang, Yalin M.D.1,. Antidepressants for bipolar disorder: A meta-analysis of randomized, double-blind, controlled trials. Neural Regeneration Research 8(31):p 2962-2974, November 05, 2013. | DOI: 10.3969/j.issn.1673-5374.2013.31.009
Sheline YI, Makhoul W, Batzdorf AS, Nitchie FJ, Lynch KG, Cash R, Balderston NL. Accelerated Intermittent Theta-Burst Stimulation and Treatment-Refractory Bipolar Depression: A Randomized Clinical Trial. JAMA Psychiatry. 2024 Sep 1;81(9):936-941. doi: 10.1001/jamapsychiatry.2024.1787. Erratum in: JAMA Psychiatry. 2024 Sep 1;81(9):948. doi: 10.1001/jamapsychiatry.2024.2327. PMID: 38985492; PMCID: PMC11238064.






Gee. Thanks for the explanation. I needed it.