Can Brain Stimulation Get Better as a Treatment for OCD?
The combination of an old medicine and rTMS may be a potent option for OCD
This has been a remarkable epoch. It's been remarkable a number or respects, not all of them good. Welcome to The Frontier Psychiatrists newsletter, a chronicle of our remarkable epoch. Times? It’s hard to know what to say about the now, broadly.
However, the science of brain stimulation has been making leaps and bounds at the very least. There are two major discoveries, in my mind, driving this improvement in what is possible. The first is the ability to replicate work originally done by individuals like Mike Fox and Sean Siddiqi, using the methodology of lesion network mapping. In short, scientists figured out how to take a functional brain scan, with fMRI, and work out which circuits were dysfunctional. They did this by using thousands of brain scans of people who that had injuries producing similar deficits. Overlapping these “similar deficit” cases, the “Connectome1” scientists could map the networks in the brain. The human connectome project was the basis of this work. The scientist, who I'm proud to work with regularly, who's driven this forward? Most importantly, Dr. Shan Siddiqi. The very same approach that helped us unlock treatment for depression has now gone on to demonstrate utility in the treatment of anxiety, the functional networks for PTSD and it's subsequent treatment, and just this past month we have networks for psychosis, and more is coming.
The ability to have a reliable and replicable methodology to address new brain problems with established and safe treatment approaches is awesome. Dr. Siddiqi's work is detangling the circuits of the brain. It offers tremendous hope.
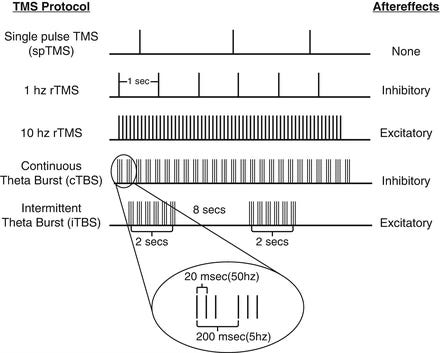
The other discovery, now replicated yet another time, is that by combining brain simulation approaches, particularly a pattern of stimulation called intermittent theta burst stimulation (iTBS), with pro-plasticity drugs like d-cycloserine, we can allow the brain to change even faster and more definitively.
This is like rocket fuel for the moon landing. Except our moon landing is help for hard to treat brain disorders. In the most recent issue of the American Journal of Psychiatry, yet another study was published demonstrating this approach is productive. I think these two lines of evidence, taken together, will allow a more effective discipline to emerge. Let me walk you through today's study:
Intermittent Theta Burst Stimulation With Adjunctive D-Cycloserine for Obsessive-Compulsive Disorder: A Randomized Clinical Trial
The trial was conducted in Canada, to determine if treatment with D-Cycloserine would augment iTBS (a pattern of TMS) in the treatment of OCD.2
Yes, attentive readers, this is the same combo of drug and iTBS stimulation as previously featured in my article about the ONE-D trial from the team at Ampa Health.
You remember, that ONE DAY protocol for depression?
The treatment we are deploying RIGHT NOW at my clinic in New York?
Yes. That one. Now, in OCD…Here are the inclusion criteria for the current study:
Eligibility criteria were men, women, and non-cis-gendered individuals 18–65 years of age with a primary diagnosis of OCD per DSM-5 criteria; YBOCS ≥20; nonresponse to at least one adequate trial of an SSRI (>4 weeks at adequate dose) or exposure-based cognitive-behavioral therapy (CBT; ≥2 months or ≥8 sessions); stable medication regimen for 4 weeks prior to and during the study; and having normal blood work. Exclusion criteria were allergy to d-cycloserine, acute suicidality, psychosis, and TMS safety criteria (substance use disorder, seizures, pacemaker or metallic implant, unstable medical condition, pregnancy or lactation).
I am a fan of these inclusion criteria. They include the medication class most relevant to the disorder! SSRIs are historically the best medicines, along with Clomipramine, for OCD) or the other gold standard treatment, which is Exposure and Response Prevention Therapy (ExRP).
This establishes a standard for “treatment-refractoriness” that makes me more likely to believe the results of this study. I have previously shared my enthusiasm for ExRP therapy, as offered by colleagues at NOCD.
They then did some real science! They enrolled subjects into 4 different groups: sham+placebo, sham+d-cycloserine, iTBS+placebo, or iTBS+d-cycloserine. This allowed investigators to tease apart the potential treatment effect of d-cycloserine alone versus the theorized combination treatment.
The study ran for 8 weeks (they were not accelerating the treatment). What they found was a huge deal:
change in clinician-rated YBOCS after 4 weeks of treatment, the primary endpoint ITT analysis (controlling for baseline symptoms) revealed a significant difference between the groups (F=9.22, df=2, 20, p<0.001) with a large effect size of iTBS+d-cycloserine (versus sham Cohen’s d=1.34 and versus iTBS+placebo Cohen’s d=1.18).
iTBS on its own would be a remarkable, game changing OCD treatment…which, of course, I’ve already published on (buried in these other large data sets, mostly). However—combining iTBS and d-cycloserine?
Even better. If it was a treatment for height, it would make you 3.35 inches taller. That is using the Muir-Skee Lo Emotionally-Corrective Equation, if you want to check my math.
This is a huge deal. This treatment works when other treatments have failed, to a huge degree. We still don’t know how this works as a first line treatment. Those studies have not been done.
If you are thinking, well, let’s go get this treatment now…it’s not that simple.
Of course, there was a shortage of d-cycloserine… that ended the trial early. Yes, it’s a national shortage. Yes, I’m working on a solution for my clinic. Yes, we already found a supplier for the drug. Yes, It is to obtain. Here is a great podcast on the topic of drug shortages, in case you are interested.
The bottom line? We have more hope for the treatment of OCD that hasn’t responded to first line treatments like ExRP. If you want that treatment, it’s available at Fermata in NYC right now.
The connectome may be defined as the complete, point-to-point spatial connectivity of neural pathways in the brain.
McGirr, A., Cole, J., Patten, S. B., & Adams, B. (2025). Intermittent Theta Burst Stimulation With Adjunctive D-Cycloserine for Obsessive-Compulsive Disorder: A Randomized Clinical Trial. American Journal of Psychiatry, 182(3), 307–311. https://doi.org/10.1176/appi.ajp.20240181





Could you comment on the validity of the DRD4-7R allel on ADHD, high risk behaviors and addictions?