Adolescent Depression: Can We Skip Oral Antidepressants?
Three new publications sets offer an option beyond drugs with a black box warning for suicidal behavior.
Adolescent depression sucks. It sucks for the adolescent. It also sucks for the parents. Worrying about your kid is absolutely the worst. Worrying about your kid feeling sad and miserable maybe an additional level of difficulty, and the absolute worst is worrying that your kid is gonna die by suicide. And yet, a plurality of adolescents are considering suicide every day, and many of them have depression.
Suicide is a major cause of mortality in youth. From 2011 to 2020, suicide was the second leading cause of death for 10- to 24-year-olds (n 5 59 827), with homicides third (50 087) and malignant neoplasms a distant fourth (18 904). In 2020, suicide was the 10th leading cause of death for 5- to 9-year-olds, the second leading cause of death for 10- to 14-year-olds, and the third leading cause of death for 15- to 24-year-olds.1
We need to get past the very depressing fact that being shot to death is the leading cause of death among children in America. At this point, much of which is in mass shootings, we can understand that this is a big problem. It's depressing to live as a kid in a country where we very clearly prioritize people having the guns to kill you versus “you not getting killed.”
After being shot to death is killing yourself, for most ages of children. So it's upsetting that the treatment for depression that health professionals can most easily reach for, at this point, are oral medications. Those same medications, as a class, have a blackbox warning for increasing the risk of suicidal ideation.
Whether these drugs increase actual death by suicide is another matter entirely, and on average, I think the answer is no. But that's not what this article is about.
It would be really nice if we had a treatment for depression in adolescents, who are so at risk for death by suicide, and are additionally at risk of feeling miserable because they're suicidal, that didn't increase the risk of the very problem we are seeking to ameliorate.
Astute readers will guess that I'm setting up the fact that this already exists. And even more astute regulators will guess that it's probably something having to do with brain simulation. Yes, readers, it's transcranial magnetic stimulation (TMS).
We have an FDA clearance of TMS treatment for adolescent depression! For readers of this newsletter, that's old news. The clearance allows for the adjuvant treatment of depression. Adjuvant, meaning “in addition.” In addition to what? We have another first line treatment for depression…That's not drugs. It's psychotherapy. Psychotherapy has a remarkable track record of effectively treating adolescent depression. So what if we use TMS plus psychotherapy instead of TMS plus medications?
How quickly can that be accomplished? For a parent dealing with a suicidal adolescent, nothing can be soon enough! But sooner is better than later. So my colleagues and I answered that question in the following publication:
Saint Neuromodulation System to Treat Major Depressive Disorder in Adolescents
And the answer is in five days…If you're using accelerated fMRI-guided TMS with SAINT.2
But not everybody has access to enough MRI, so could it be done reliably with other transcranial magnetic stimulation devices? Perhaps with devices that are already broadly deployed? And, not to keep you, dear readers, waiting, but other colleagues and I answered this question also. Yes, we can very much get adolescent depression to remission. And we can do it in large populations, with 1200+ patients in the real world, now published:
Safety and efficacy of Deep TMS for adolescent depression based on large real-world data analysis
But, Dr. Muir, tell us, how effective is this? Is it more effective than the drugs you're asking us to forsake? The answer is definitely yes. It's both safer and more effective.
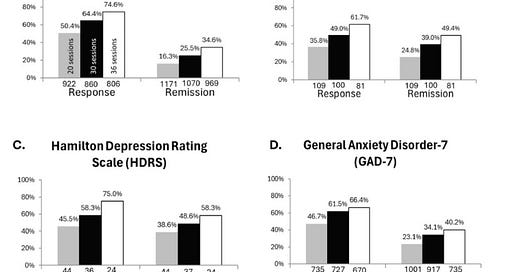
After 36 sessions the response/remission rates were HDRS: 75.0 % / 58.3 %, [and on the self report] PHQ9: 74.6 % / 34.6 %.3
So the question I'm gonna ask, all parents, and all pediatric specialists everywhere, why are we still treating adolescent depression with a combination of medication and psychotherapy when we could be using psychotherapy alone as a first line, or psychotherapy plus TMS if the depression is bad? Why are we getting anywhere near drugs with a risk of increased suicidal behavior, not to mention weight gain and other problems, when we could be using something with a much higher likelihood of getting kids to not have any depression anymore?
I don't think we should be prescribing oral antidepressants as a first line approach in adolescent depression, because it's higher risk, less safe, and less effective.
Now, send this article to your health plan to make sure they cover the treatment.
If you have a young person in your life who needs treatment for depression, I work at a series of centers that provide the treatments I write about. Get more info …
or…
Liwei L. Hua, Janet Lee, Maria H. Rahmandar, Eric J. Sigel, COMMITTEE ON ADOLESCENCE, COUNCIL ON INJURY, VIOLENCE, AND POISON PREVENTION; Suicide and Suicide Risk in Adolescents. Pediatrics January 2024; 153 (1): e2023064800. 10.1542/peds.2023-064800
Cook, I. A., Carreon, D. M., Solvason, H. B., Bota, R., Barbour, T., Pottanat, R., ... & Bentzley, B. (2025). 180. Saint Neuromodulation System to Treat Major Depressive Disorder in Adolescents. Biological Psychiatry, 97(9), S169.
Roth, Y., Tendler, A., Pell, G. S., Tripp, T., Yam, P., DeKeyser, D., ... & Hanlon, C. A. (2025). Safety and efficacy of Deep TMS for adolescent depression based on large real-world data analysis. Psychiatry Research, 116567.




We are not just shifting the conversation; we are reframing the entire lens on suicidal thoughts. We are cracking open space for people of any age to feel seen without shame and to find possibilities in their darkest moments. We are taking the most intense human pain and giving it language, dignity, and a path forward. All in the hopes of not losing one more. Will you join us? SHARE THIS WITH PEOPLE WHO CARE ABOUT PEOPLE.
https://open.substack.com/pub/paintopossibilities/p/an-invitation-to-be-part-of-something?utm_source=share&utm_medium=android&r=2at1yi
First line treatments need to be benign. Adolescents don't all go on to develop more serious disease but iatrogenesis is very real. Using safe first line treatments and monitoring for poor response is the warning system for emerging disorder. Its the model in other branches of medicine, why is psychiatry so slow?