A New Treatment for PTSD Based on Brain Science
Also knowns as the "human connectome project, for dummies."
The Frontier Psychiatrists is a health-themed newsletter. Today, I will explain some of the science behind the healthcare I provide. I work with brain scans, obtained via a magnetic resonance imaging (MRI) scanner. These scans allow us to understand how the brain is structured. It also can illuminate how the brain talks to itself. We use these scans to guide brain stimulation treatment most frequently with transcranial magnetic stimulation (TMS). It’s best to start by acknowledging those whose work made precise treatment with brain stimulation possible. Mike Fox, M.D., Ph.D., is a physician-scientist at Harvard. He is one of the individuals behind the human connectome project.
What is behind this ambitious project? We all have brains; they're made up of neurons and supporting cells (glia). When part of the brain is more active, it pulls more oxygen off hemoglobin—on which it had been hitching a ride—in the blood. This happens when that region of brain needs more energy. The MRI scanner allows us to take a more extended brain scan, beyond a still picture. We can see blood flow to active tissue. This is measured by increased demand for oxygen, which is pulled off of hemoglobin, which in MRI research is called BOLD signal change. The more active a part of the brain, the more the BOLD signal changes on a scan. In the MRI scanner, these changes in the BOLD signal could highlight changes occurring simultaneously in different parts of the brain. The scientists surmised that those simultaneous changes indicated that brain circuits were working together.
When activity in one area of the brain and another area of the brain went up and down in the same rhythm, this is dubbed functional connectivity. It doesn't mean these areas are physically connected in some way; although that may be the case. It means they're working together. It's like a drummer and a bass player in the band. They don't have to have a cable between them to be work as a rhythm section. Similarly, a jazz band's piano, bass, and drums have an underlying rhythmic purpose. They function as one rhythm section, together. They are synchronized to support both rhythm and harmony, which are the same thing at different time resolutions, as it turns out:
Mike Fox and colleagues had an idea. What if we looked at the brain scans of people who had had injuries and tried to understand the deficits observed after these brain injuries? What if the changes in the BOLD signal indicated a functional connection—the brain’s answer to being in tune? And, of course, What if we could retune an out-of-tune brain?
When the history of how we healed psychiatric illness is written, it will also features my colleague Shan Siddiqui, M.D., a neuropsychiatrist at the Harvard Brain Science Initiative. His most recent contribution follows in the footsteps of Dr Fox:
The most straightforward example of this is post-traumatic stress disorder. Vietnam veterans sometimes got brain injuries from shrapnel to the head. Some of those individuals ended up not developing post-traumatic stress disorder (PTSD). They were protected from that problem in the brain.
We have here a natural experiment! Areas in the brain that are taken out randomly by shrapnel. With a physical brain injury, we know where it happened. The investigators looked at this library of brain injuries — some of which appeared to protect against post-stress disorder.
The same mapping approach has been instructive in understanding depression, anxiety, mania, and other conditions. We have been able to look at individuals with various injuries and surmise that what we were looking at was a break in a circuit. The theory is that different areas of the brain are functioning as one circuit, and if you break it anywhere, it won't work.
The idea behind the human connectome project was to map those brain circuits—connected circuits, borrowing from the human genome; they added -ome to the end of the name. They are starting with data from lesions (a.k.a. damage): If one person has a lesion in the left front and another in the right rear but they create the same deficit, maybe they're part of the same circuit?
The next step would be to look at an MRI scan of somebody without that brain injury and see if functional connectivity patterns can tell us anything useful. Suppose we have a PTSD circuit, as hypothesized by lesion information. In that case, it should be possible to stimulate the neurons in that circuit noninvasively to treat PTSD in the same way that accidental brain injuries protect against PTSD.
It would be some very exciting science, not to mention wildly popular medicine, if this approach works to treat PTSD. Today, in the prestigious journal Nature Neuroscience, the first academic paper on this topic was published today! Not only have Siddiqi and his team mapped a novel PTSD circuit, but doctors at Acacia Clinics, including Frontier Psychiatrist David Carreon, M.D., used this brain map to treat PTSD. The following is how Acacia’s team explains it:
The research, based on data from 193 Vietnam veterans with penetrating traumatic
brain injuries, shows that damage to brain areas connected to the amygdala—the
brain's "fear center"—can protect against PTSD. By mapping these lesions to a specific brain circuit, the study provides a blueprint for targeting PTSD with non-invasive brain stimulation techniques, such as Transcranial Magnetic Stimulation (TMS).
David puts is plainly:
“This is one of the first times in the history of psychiatry that we successfully designed
a treatment,”
— Dr. David Carreon
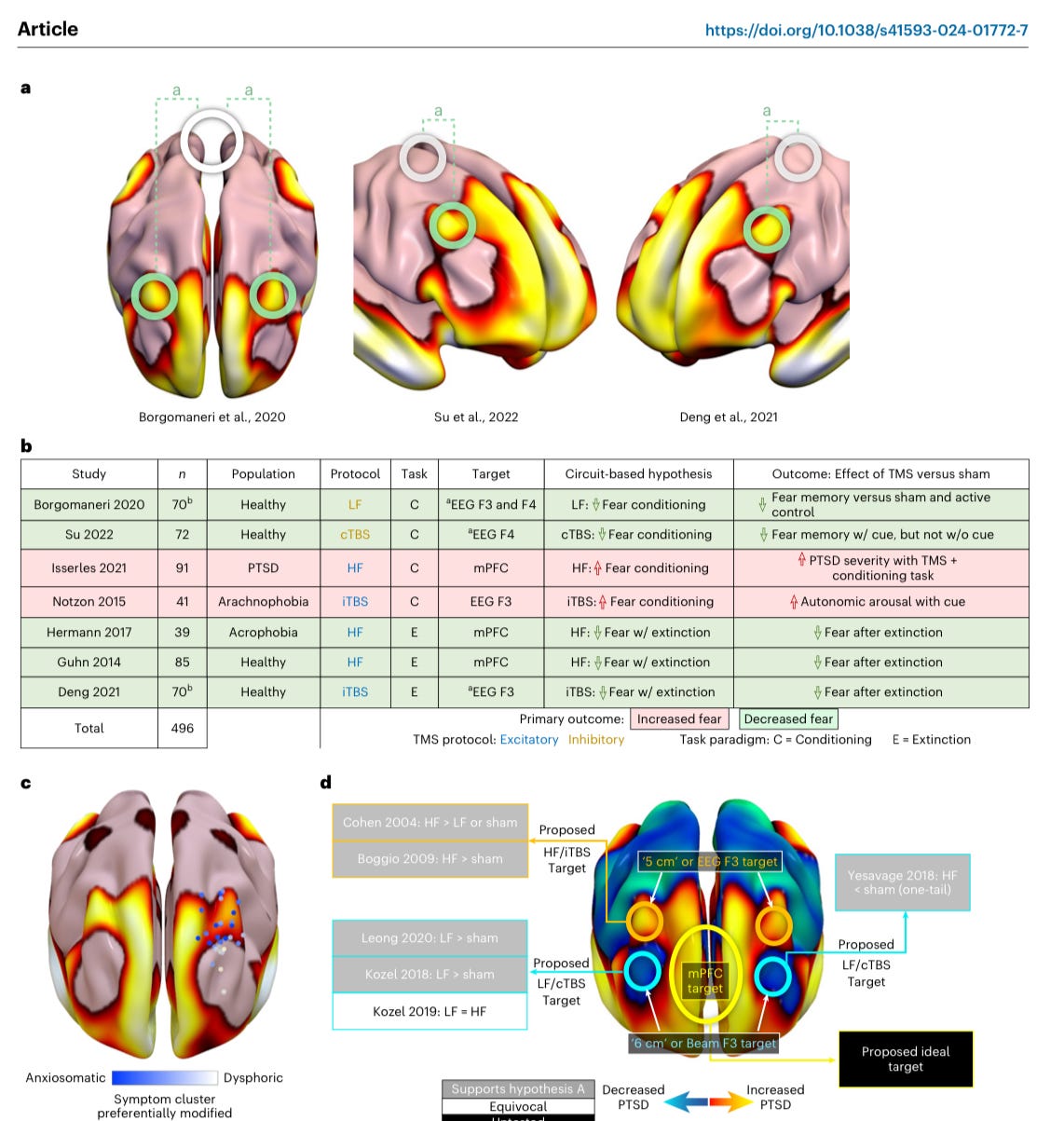
We used science to answer a mechanism question about why people might be suffering from PTSD. We used science again to design a treatment for that suffering. It worked. This is what a better future looks like. Now, here are some science-y pictures of a brain to add convincingness to this article:
That is the series of images that demonstrate where the lesions were in the brains of the individuals we were looking at. Those boil down to the full PTSD circuit below:
This science led to our ability to generate a target for stimulation:
Next, we were able to treat an individual, as published, with the treatment, and have them improve. In just five days. This is a triumph for translational neuroscience.
Your author, Owen, happen to be on the team call when we discussed the deployment of this novel target for the first time. And we haven't stopped since then. More publications will be forthcoming. However, the ability to get innovation to patients quickly is the remarkable story here.
This is a land speed record in bench-to-bedside translational neuroscience. We discovered something in science, and patients were treated before the paper was even published.
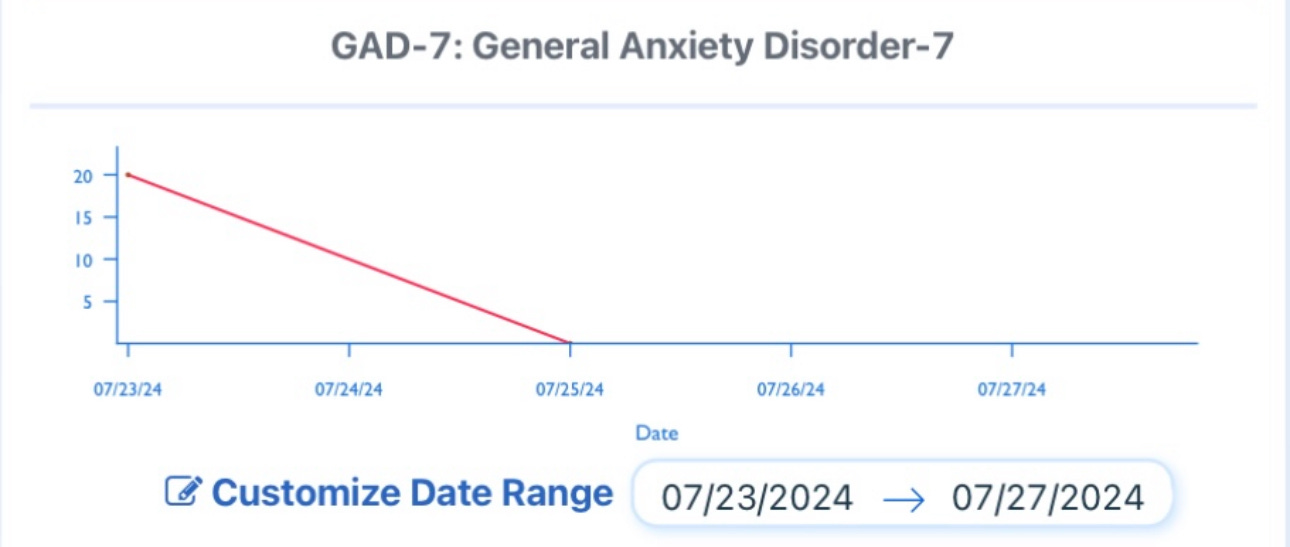
We subsequently replicated the approach in my clinic —Fermata—in New York as well, using a different stimulator technology based on the underlying science, and this is what those outcomes look like:
Yes, that's an anxiety going from the maximum score to zero in three days. But this was about PTSD, so how did the individual do on their PTSD rating scale? That took longer, it took five days of treatment:
But you'll notice the depression got better in just three days as well.
This was all before the paper was even published. The traditional time for a research finding to reach general clinical practice is 17 years, on average. Getting science into the clinical setting before the paper is even out? That may be a first.
Welcome to a future of less suffering; it's here now. Other systems need to catch up, but science is not the rate-limiting step this time.








This sounds tooooo good to be true!!!! But I do hope it's that good and that true. I for one I'm sick with the constant refrain of trauma-informed care that is so vague and woowoo sometimes and doesn't achieve anything near what you are showcasing in this novel treatment. I mean, could we have the first actual cure in psychiatry?!!!
amazing