Today, The Frontier Psychatrists welcomes back my friend Ben Spielberg. He's been a reader for a long time and has contributed to the newsletter in the past. It was on Clinical Trial design, a perennial favorite around these parts.
With only light edits, what follows is his work, narrated by me, for the Audio Version.
I would invite you to the live class today on working as an out-of-network provider, but it sold out last night, so you'll have to wait for the next one.
My prior article on Spravato is available here.
The year is 2024. OpenAI has just launched its latest update to ChatGPT, promising more natural and less artificial-sounding language. Donald Trump has won the nomination for President of the United States. Another chain of ketamine clinics has engaged in a corporate reorganization. There is conflict in the Middle East. Are we sure that we're not living Groundhog's Day?
I am the founder of Bespoke Treatment, an integrative mental health facility with multiple locations that has at times been referred to as a "ketamine clinic." I have also seen countless so-called "ketamine clinics" sell for pennies on the dollar and go bankrupt seemingly overnight. In this case, Numinus, a company that was publicly traded in Canada and owned a number of psychiatric clinics specializing in ketamine in the US and Canada, has sold its clinics to Stella (a company that has stealthily become one of the larger mental health providers in the country and is the first to bring the awesome SGB treatment to scale). It's not the first time this has happened. It's not the second, nor the third, nor even the fourth time this has happened. But yet, the common consensus is that ketamine clinics are a cheap, easy business with recurring revenue. So, what gives?
Figure 1. A reddit user asking anesthesiologists if they should start a ketamine or Botox clinic for easy cash on the side. Does this make you feel gross? Should it?
The Ketamine Clinic Model 101
The most basic outline for a ketamine clinic is as follows: a provider rents an office space with, on average, five or so exam rooms. They buy equipment for infusions like a pump, catheter, needles, and syringes. They buy some comfortable recliner chairs. They hire a receptionist to answer phones, field patient questions, charge credit cards, and handle medical record requests. They hire a nurse to insert the IV, monitor vital signs, check blood pressure, juggle multiple patients at once, and make sure the ketamine is flowing into patients’ veins unencumbered. Two SKUs are typically offered: ketamine infusions for mood, which last approximately 40 minutes, and ketamine infusions for pain, which last for up to 4 hours. Zofran is offered for nausea, and some clinics have fun add-ons like magnesium or NAD. An average mood infusion costs around $400-$500 in a medium cost-of-living area, while mood-infusions can run up to $700 in a higher cost-of-living area. Some clinics offer package discounts if patients buy six or more upfront, which helps with cash flow for the clinic (cash now is better than cash later, of course).
A Note on Scope of Practice
The first wave of ketamine clinics was started mainly by providers who were not mental health specialists. Instead, they were owned by anesthesiologists, ER physicians, and sometimes CRNAs. These providers were especially experienced with ketamine in hospital settings, as well as setting up infusions. Psychiatrists, on the other hand, do not usually order infusions in outpatient settings, and very few had actual hands-on experience with ketamine in practice. That being said, there are a number of variations to the model above: psychiatrist-owned ketamine clinics would often prefer to use intramuscular injections in lieu of infusions, but 2-3 injections would have to be given during a single session for mood and pain sessions were out of the question. Other ways to save costs might include having an EMT do the actual injections (this is highly state-dependent), asking nurses or MAs to work the front desk, or working a full-time regular doctor job. In contrast, your nurses run the actual ketamine services via standing orders, a written document that details routine and emergent instructions for the clinic.
Some clinics offer full evaluations prior to rendering treatment, but many offer a simple brief screening on the phone to check for contraindications before scheduling a patient for their first session. The clinics owned by psychiatrists have historically been a bit more thorough in terms of the initial psychiatric evaluations, given that they can actually perform initial psychiatric evaluations within their respective scope of practice. Sometimes clinics may have therapists on-site who can render ketamine assisted therapy (meaning, therapy occurring concurrently) for an additional $100-$300. Otherwise, there is not much decision-making that goes on— other than deciding on medication dosages. Most infusions start off at .5mg/kg of body weight, which is by far the most evidence-based dosage. In practice, most clinics increase dosage every session because even though ketamine is considered to be a weight-based medicine for anesthesia, there is thought to be a “sweet spot” of dosage for everyone, if one can imagine an inverted U shape curved, where the ideal dosage for each patient is at the tippity-top of the inversion. Dosage increases are highly variable depending on the clinic: some have a maximum dosage, some will only increase a certain percentage, and some may even use standardized increments (e.g., only offering dosages in increments of 50mg). A typical series of infusions is 6-8 over 3-4 weeks, followed by boosters as needed.
Fool’s Gold
At first glance, the business model seems fantastic. As a cash business, there are no AR issues, no third party billing companies to deal with, and no prior authorizations to fight over. Sure, the cost is high, but it’s not that high compared to many other healthcare services. Since the benefits fade over time, a ketamine clinic has built-in recurring revenue from patients every week, month, quarter, or year – it’s like a subscription business! Ketamine is trendy and sexy; TV shows like White Lotus mention it, and ravers from the 90’s recall it with great fondness. Unlike SSRIs and psychotherapy, ketamine works for depression fast. It’s amongst the fastest treatments for depression that we have today, and there are a lot of depressed people. It can help someone out of debilitating depression in 40 minutes. It has none of the un-sexy side effects of SSRIs like sexual dysfunction, gastrointestinal discomfort, or uncontrollable sweating. Instead, it has sexy side effects: euphoria, hallucinations, and feelings of unity with the universe. Also, unlike SSRIs, it helps most people who try it. It really is an amazing treatment, and I often feel grateful that my clinic is able to offer it to patients in need
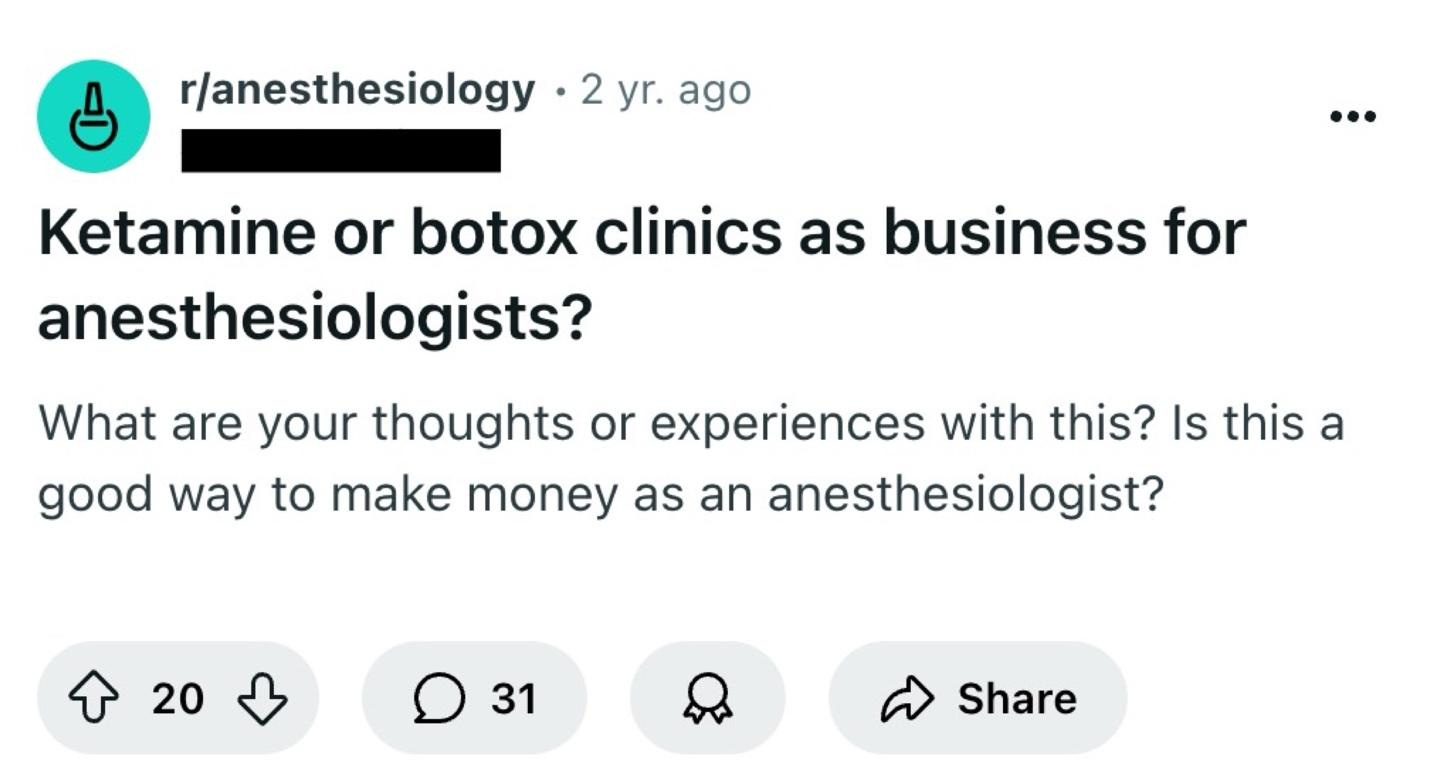
Figure 2. Most business-savvy reddit user.
Supply and Demand… or Something
Mood disorders disproportionately affect individuals who are of lower socioeconomic status compared to individuals with a lot of disposable income. Of course, wealthier individuals are no more immune to mental health disorders than anyone else, but the main target market that benefits most from ketamine just do not have the means to afford it. They don’t have $3,000 to burn on yet another treatment that may or may not work. Often, the patients who could really use a series of ketamine infusions cannot scrounge enough money for a single infusion, let alone a whole series and prn boosters. However, there should be enough depressed people with cash to throw around out there… right?
Wait, Isn’t That A Horse Tranquilizer?
Of course, ketamine clinics can find more patients via marketing and advertising. However, I’ve found that many medical doctors who see this population, like primary care providers, are not up to date with the research. When I first launched my company, I used to go door-to-door to medical buildings in Santa Monica with cookies to speak with them about advancements in interventional psychiatry. I cannot count the number of times that I was laughed out of each office; referring providers are risk-averse, and the perception of ketamine has traditionally been poor. Medical doctors would exclaim, “Of course people feel better; you’re getting them high,” and lament that I was administering a drug thought to be highly addictive. Psychotherapists, who would also be fantastic referral partners, generally refer to psychiatry, but it’s less common for them to refer to specific treatments. Nowadays, psychotherapists who are particularly invested in ketamine can sign up with venture-backed companies like Journey Clinical and render their own ketamine-assisted psychotherapy with some prescriber supervision. The issue is that despite the media attention, people with depression don’t read innovative health newsletters, nor do they review papers in scientific journals. They rely on information from their psychiatrists, medication management providers, and psychotherapists. If they are not told that this is an option for them, they won’t hear about it without ad spend. Oh yeah, and there is a major issue with ad spend: the word ketamine itself is a restricted drug term, and legitimate clinics routinely get banned from Google and Meta for mentioning it, which makes digital advertising more difficult than it would be for any other legitimate service.
The Matthew Perry Effect
Ketamine is very desirable for some patients (unfortunately, sometimes the patients who want it most are frankly the worst candidates for it), but I’d wager that the majority of patients who need it are kind of scared of it. They want to feel good, they want relief from depression and trauma, but it’s a weird thing to do a drug that is a horse tranquilizer and also an anesthetic in a reclining chair in a medical office that tricks your brain into feeling like you’re dead for a little bit. It’s kind of far off from acupuncture and more traditional alternative medicine. There is certainly a non-zero addictive potential that needs to be carefully weighed, it’s not a particularly comfortable experience for many patients—especially those with a history of trauma—even if it helps after the experience is over. Additionally, the famous actor from the most famous show in the world, who was deemed to have a cause of death relating to ketamine, isn’t exactly helping mass adoption. Overall, this just makes marketing and advertising even more expensive, because a) the majority of referring providers are skeptical, b) patients can’t pay for it and c) patients who can pay for it are cautious.
Disruptive Business Models
In the model I’ve described above, there are 3 sets of cost centers: rent, staff, and marketing. In some areas of the country, rent may be negligible, and in others, it is quite high. Like an owner-operated restaurant, if a clinic is owned by a company that is not a clinician, they have to find one and pay for one. Venture-backed companies like Mindbloom, Better U, and Joyous have also created entire businesses on the back of the COVID-era controlled substance waivers, whereby they send patients ketamine tablets and/or lozenges directly through the mail. Unlike the clinic model, they don’t have rent to pay, and since national marketing campaigns are often cheaper than hyper-local brick and mortar campaigns, they are able to find new patients at lower acquisition costs compared to their clinic counterparts. Some patients do extensive research before treatment and only want to find IV clinics that offer specific dosages, but many are fine with the cheapest ketamine possible, and would prefer to pay as low as $150 for an entire month compared to $3,000.
Figure 3. Did you sign up for a discounted ketamine subscription on Black Friday after purchasing a new flat-screen TV?
Spravato: Coming In Hot
Johnson & Johnson’s branded esketamine (note the prefix es) is on track to reach coveted “blockbuster status.” While it was FDA approved for Major Depressive Disorder in 2019, it took some time to catch on for a number of reasons including skepticism that the added es only added to pharma pockets and didn’t actually work, health insurance companies taking time to decide on what their medical necessity criteria should be, and social isolation due to COVID-19 being a thing. My clinic has become one of the larger Spravato providers in the Los Angeles area, and while we still offer ketamine infusions, our infusion census has decreased by over 70%. The scenario is this: a patient with severe depression comes in to see us, they’ve heard about ketamine, but they find out that Spravato is covered by insurance for a $20 copay. Maybe ketamine has slightly better efficacy (which, in my opinion, is really just a function of being able to adjust dosage). Still, patients would prefer paying a lot less money to receive almost-the-same benefits.
Death By A Thousand Sticks
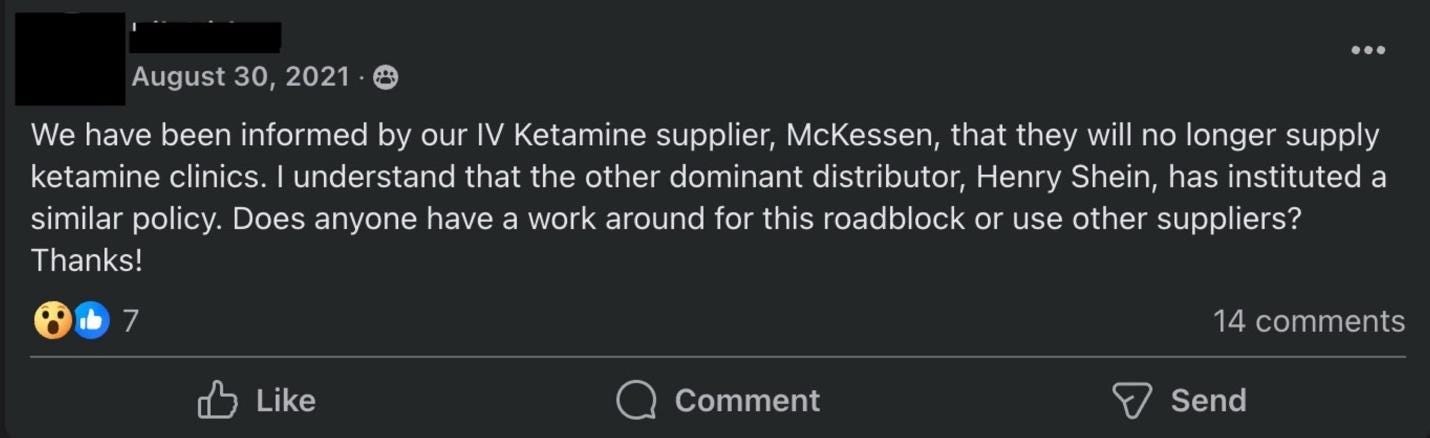
There are a number of other issues with the model that become problematic, especially at scale. Large medical distributors like McKesson and Henry Shein have instituted CYA policies, limiting ketamine sales to licensed anesthesiologists. Medical malpractice carriers alike have followed suit, requesting detailed addendums from providers regarding their ketamine training or flat-out refusing coverage for anyone who isn’t an anesthesiologist. Since controlled substance manufacturing is directed by the DEA based on their own predictions, it’s not uncommon for ketamine to go on shortage for weeks to months at a time. There are a myriad of problems with the model of point solutions which have been detailed here already, but in short, the old adage rings true: if all you have is a hammer, everything looks like a nail, and if all you have is ketamine, everything looks like a juicy vein. But while ketamine is a highly efficacious treatment, it’s not the best treatment for everyone, and patients can become downright dysregulated after ketamine, which a clinic in this model just can’t handle adequately at scale. And ultimately, methods to do everything cheaper don’t work out that well. For example, putting multiple patients in one room may seem like a good idea, but it is ultimately not conducive to the actual ketamine experience. Any sort of vertical integration also adds an insurmountable amount of complexity, like starting to offer Spravato or TMS, because now they have to start accepting insurance, become in-network, manage billing and AR, and so on. Depending on location and the clinic set-up, they also require specialized providers onsite.
Figure 4. Supply chain issues abound.
Insurance Issues
Some patients try to be well-informed. They, rightly or otherwise, don’t believe everything they hear from their providers, so they call up their health insurance companies and ask. They just call the phone number on the back of the card and ask the representative if ketamine infusions are covered. Undoubtedly, the representative says yes—even though many insurance companies have published guidelines that explicitly deny any coverage for ketamine for a mental health disorder. These patients come in frustrated, distrustful of their providers and reaffirms their belief that ketamine clinics are just cash grabs. Even if one manages to obtain a coveted insurance contract for ketamine, like Ketamine Wellness Centers had with the VA, it kickstarts cashflow and complexity issues that scale should sort out, but ultimately doesn’t because of the aforementioned issues above.
Overall, it is possible to have a successful ketamine clinic in 2024. Still, it isn't easy due to market conditions, the population served, and the ever-changing landscape of mental health treatment. While many successful clinics exist today, the wheels tend to start to fall off when scaling, where all of a sudden, a clinic’s reach has surpassed its captive population. Otherwise, it becomes a series of continual cost-cutting until there is nothing left to cut… save for the business itself.
Ben Spielberg is the Founder and Chief Executive Officer of Bespoke Treatment, a comprehensive mental health facility with offices in Los Angeles, CA, and Las Vegas, NV. He is also a PhD Candidate in Cognitive Neuroscience at Maastricht University.
For more on psychiatric medications, buy my book Inessential Pharmacology. (amazon link).
For pieces by other TFP contributors, follow:
Alex Mendelsohn, Michelle Bernabe, RN, @Psych Fox, Carlene MacMillan, MD, David Carreon, M.D., Benjamin Lippmann, DO, Awais Aftab, Courtny Hopen BSN, HNB-BC, CRRN,
and many others!





This was quite insightful into the business side of things!
This is such a great breakdown of the state of affairs in the ketamine industry!