I Solved "Prior Authorization" with this One Weird Trick
Thinking like a payor to solve the problem
I had insomnia last night. Documented below:
And…cracked a (conceptual) nut. No, it wasn't about not sleeping. It was about how to solve prior authorization.
A little background, for general audiences. Big Health companies, which we have traditionally referred to as “insurance” companies do a heck of a lot more than insure. What started out as a way to make hospitalization not devastatingly costly grew into the giant corporate behemoths that we have today. Take a minute with the pluralization of the word behemoth.
The original behemoth was of course a giant land creature first mentioned in the Bible in the book of Job. It turns out, behemoth was the first of God's creations. It's supposed to be the biggest thing. It's not supposed to be plural. Here's what it says in the Bible (Job 40:15-19):
“Behold, Behemoth, which I made as I made you;
he eats grass like an ox.
Behold, his strength in his loins,
and his power in the muscles of his belly.
He makes his tail stiff like a cedar;
the sinews of his thighs are knit together.
His bones are tubes of bronze,
his limbs like bars of iron.
He is the first of the works of God;
let him who made him bring near his sword.”
However, it's possible that you don't get everything right on a first pass. It may be, although God made a big one first, the scale of behemoth could be improved on? That ambition, presumably, is how we got UnitedHealth Group. I’ve specifically used Behemoth’s aquatic partner-in-crime, Leviathan, as an example more than once before.
Prior authorization is a policy where an insurance company which pays for medical care can require plan members to ask permission before they get specific medical care. If you think what insurance does is control costs, it would make sense to have prior authorization be part of that rubric. What if somebody wants an unnecessary surgery? Surely, Insurance shouldn't be forced to pay for just anything. It's worth mentioning that there are some systems within US healthcare where prior authorization plays absolutely no role. Medicare, for example. It's either a covered benefit or it's not, but you don't have to ask the government permission get any medical care under Medicare. They control cost by controlling what is covered. Medicare also, although it has a rationale to want to control overall costs, has no rationale to want to control individual patient level medical decision-making. Big health companies very much do. They're not actually in the business of controlling costs. They are the business of maximizing profits. The way you maximize profits is you make a fixed percentage of profits on a total overall number of healthcare dollars spent. This is called the Medical Loss Ratio, and everything in the behavior of health is determined by maximizing this absolute value of this number. The problem for Big Health is if they pay out too much money, they don't get to keep as much in profits. Thus, the ideal world (for big health) is to have the option to pay or not pay just about anything. They want to be able to pay as much as they possibly can, but not a penny more. Insurance doesn't want to control costs. They want profits. That is their fiduciary duty to their shareholders. Controlling costs is, to repeat myself, pretext ONLY. When we get angry at denials of care as a locus of public rage, we miss the point—it’s not about denials writ large, it's about WHICH denials…and the billions of paid claims that dance with denials to make such remarkable financial statements for shareholders.
This creates some perverse incentives. For example, you'd really desire to limit spending that could reduce the overall total cost of care, because that would reduce the fraction of that overall spending that can be profits. But payors can't simply not cover great medical care! Payors can, however, force people to ask permission for any medical care. Ideally, you'd want to obtain prior authorization on literally everything, or at least the vast majority of things, that would run the risk of driving down the total cost of care. Again, Big Health isn’t in the cost control business. It's counter intuitive!
None of this is a good look, thus the best way to institute this regime is to create uncertainty. From a business standpoint, it should be stochastic, impossible to predict, and relentlessly efficient at increasing the total cost of care. You always want the option to not pay, because profits. Prior authorization has become the primary mechanism by which this optionality on paying for healthcare in such a way that profits are optimized is preserved. Other systems handle this through limiting covered benefits, wait times, rationing, phantom death panels, etc, but none of those predictable mechanisms serve the additional purpose of maximizing spending. Those mechanisms predictably limit spending, which is the opposite of the point for Big Health.
The level of absurdity here is such that a colleague recently made a video on TikTok describing her experience as a oncologic surgeon in the middle of a breast cancer resection and reconstruction, who is paged by UnitedHealth Group while she was in the operating room. She is forced to scrub out of the surgery… to justify the medical necessity of the hospital stay for the patient after the operation that again, the surgeon was in the middle of performing when UHC urgently paged her out.
Going in out of an operative theater is not trivial— the scrubbing process is quick, but it's not that quick, you really do have to ensure antisepsis! UnitedHealth Group has to ensure no such thing, and they can, over the magic of the telephone, demand our attention— lest our patients are punished with life altering hospital bills that we can't even discuss with them because they're under anesthesia at that very moment.
It's at this point that I'll remind the audience that behemoth was originally introduced in the Book of Job. At least he was able to provide informed consent for his suffering to the Lord, as peri-suffering anesthesia wasn’t a thing, yet.
Denying care is one trick, but having the option to deny care, and forcing us to take additional steps in the midst of sickness and fear, lest we may be denied care? That's a whole new kind of ordeal. The uncertainty is both part of the point of the product that is prior authorization, as well as part of the anxiety and stress of dealing with American healthcare. Everything's a fight. Physicians have been pushing back on prior authorization with very little success. We tend to be a compliant lot—very Book of Job of us. Why, oh United, hath I been so unjustly Paged? The surgeon above? She didn't just tell the health insurance company to go f- itself. From the standpoint of the safety of the patient, I don't know that I would've scrubbed out of a surgery. I also don't know our modern Jobs know what they're getting paged for when they're being asked to scrub out to answer the urgent page. Heck, the communication is presumably made overhead like the voice of the Lord itself!
Big Health companies—which we used to think of as insurance companies prior to this article— are using prior authorization to maximize their profits. I don't think they're gonna give it up without a fight. Thus, I have a simple suggestion for a legal solution that will allow prior authorization to remain perfectly intact, while making it harder for Bit Health to use this solution promiscuously. Are you ready for my suggestion? Please press 1, or continue reading.
All requests for prior authorization need to be communicated by a licensed physician (on the part of the Payor) in person. That's correct. No change to the current rules or standards, but 100% of request for prior authorization of medical care needs to be done by a licensed doctor, standing, eye to eye, in the same room with the attending physician managing the patient.
If you want to obtain prior authorization, send somebody in person to ask me. Someone who's got the actual Medical Licence to understand what I'm talking about, and pay for the plane ticket.
I don't think this would be a very popular job among insurance company doctors. I think it's likely they would run out of physicians willing to get in a plane just to go meet their colleagues and demand an explanation. We don't have to change anything in the language about prior authorization, we just need to make it endlessly painful to request. If it mattered enough, they could put somebody on a plane. Or they could staff hordes of additional doctors in major urban areas all across the country and dispense them to go argue with their colleagues about whether things will get paid for. At least they'd have to look at their colleague in the eye. No more faceless phone calls, no more effortless denials. Every denial of care would have to be communicated between two licensed physician colleagues looking each other in the eye.
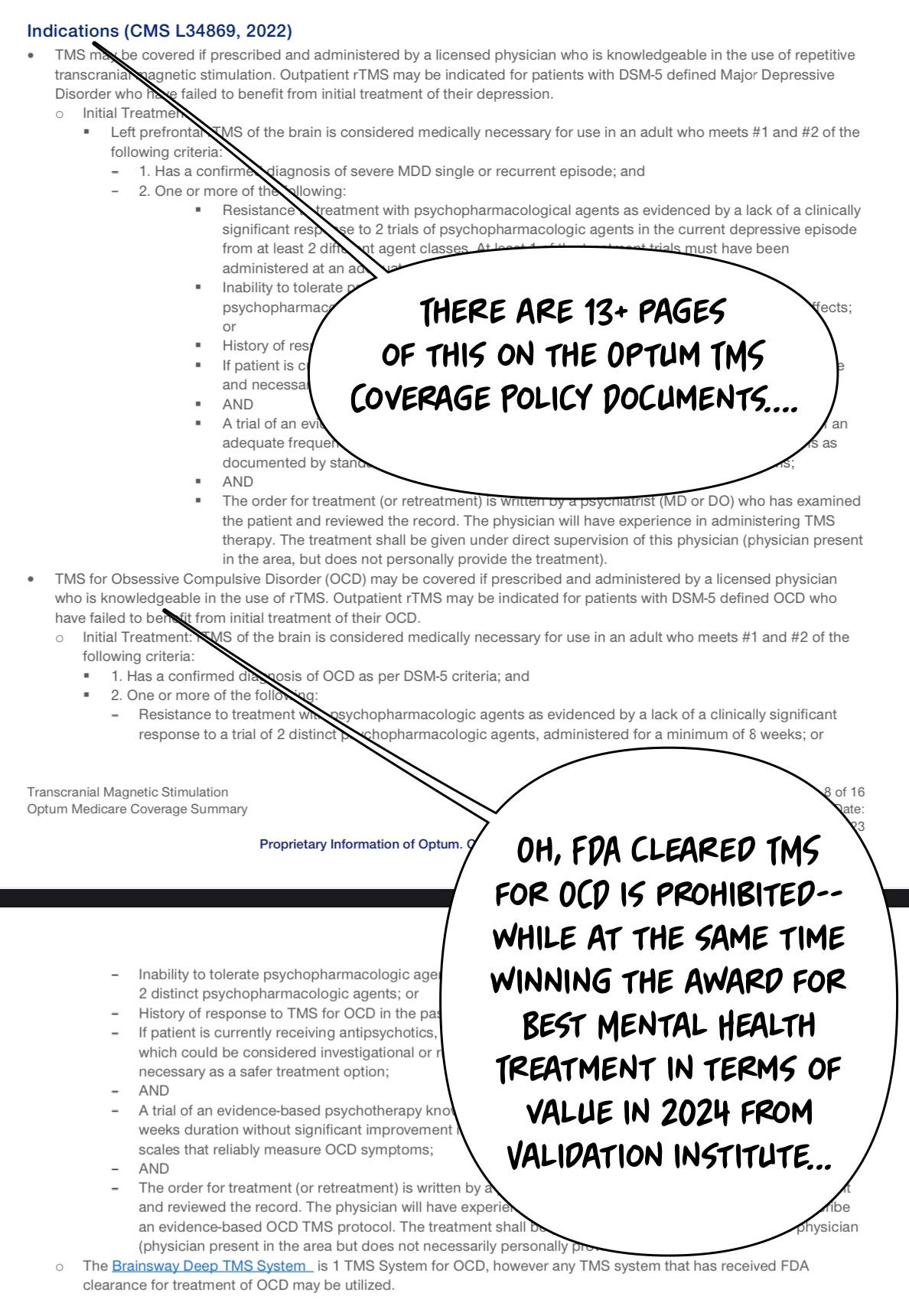
I think this is a really good suggestion. It is, of course, my suggestion. Of course I think that. It was inspired by the theoretically reasonable requirements, like having on site near-ACLS level medical care supplies available in outpatient mental health clinics (such as supplemental oxygen), or the onerous requirements used to deny rTMS care for years:
Turnabout is, I am told, fair play. Thus, without resorting to fancy word play, I hereby advocate for a simple “tell me to my face” standard. All prior authorization requests and denials must be communicated in the same manner as the care to be delivered. If it’s telehealth, denials are acceptable by zoom. If it’s in-person care, the review and denials must be face-to-face and in person and in the setting where there care is to be delivered. This benefits rural settings, for example, by making it more onerous to go all the way to the sticks to deny care personally! Oh, and all denials need to be delivered by reviewers board certified to perform the procedure denied, too. And licensed in that state. With active med mal coverage. And admitting privileges. And an active DEA license.
Your move, Big Healthcare. I look forward to discussing… in person.
Join us tomorrow in San Francisco between 6-9pm for Rapid Acting Mental Health Treatment 2025.



I don't just like this idea I LOVE THIS IDEA!
I believe this has the potential to get the problem 'alleviated' and not sorted, ofcourse.
But I presume a MAJOR pushback from the Big Health / Insurance Sharks out there simply because it translates into a ton of financing on their end which they won't make profit out of.
They would drag this to courts and fight it but ultimately if all providers show a united front in terms of legal optics, this might well push through!
Always pays out to be an optimistic.