Are Brain Circuits Driving Depression?
The remarkable progress in brain network mapping unlocks another secret of effective depression treatment
How are the care of depression and surgery interventions similar? It's about where you intervene! The first version of this hypothesis demonstrated in a randomized control trial was done by Ellie Cole et. (Along with senior author and future Nobel prize recipient Nolan Williams, M.D.), in the SNT trial1, in which they demonstrated that use of a “movie of the brain” (fMRI) generated target led to remarkable remission rates of major depressive disorder in SAINT2 treatment for depression—79%!
These data were replicated again, in a large-scale post-marketing study of SAINT, over a longer time scale—with yours truly as an investigator on the trial (note: the CGI-I is a clinician-rated measure of improvement):
At follow-up visits, percentage of participants scoring ≤2 on the CGI-I were 55% at 1 month, 55% at 3 months, 55% 6 months, 62% at 9 months, and 70% at 12 months.
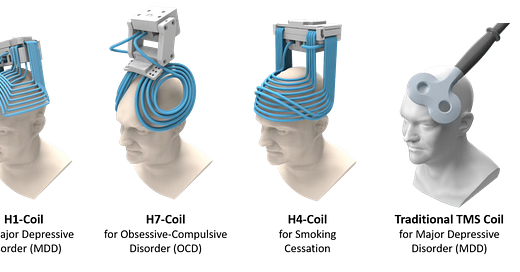
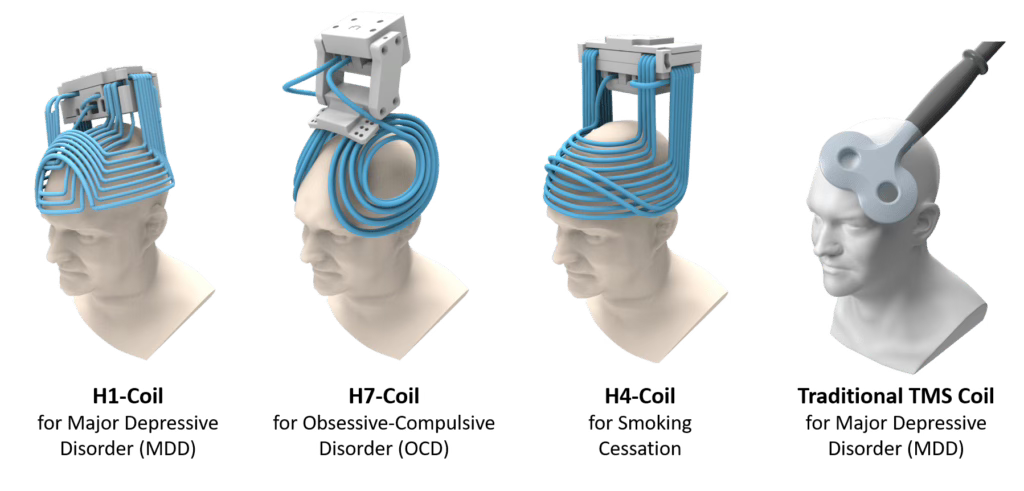
The SAINT technology requires neuronavigation with functional MRI—that's the special sauce, getting a very focal stimulator to just the right spot. However, individuals following “the space” are aware that there are other ways to simulate the brain. Just staying within TMS, you can remember that not only do we have awkward paddles, we have even more awkward-looking helmets. Inside those awkward-looking helmets are complex coil arrays that stimulate vastly more brain than a one cubic centimeter area, which is what figure-8 coils accomplish.
These H-coil systems were developed using your tax dollars at NIH, in the before times. Way back when, I’m told, tax dollars funded health research. Looking back nostalgically on those innovations, we are reminded that it's possible to stimulate wide swaths of the brain all at once!
With massive areas of the brain stimulated, could it possibly matter where those H-coils are placed?
Astute readers recognize questions like that? They are setting you up! Of course it matters! You just need the data set to answer the question! Enter the bastion of research and advancement that was also funded in the before times—yes, I'm talking about Harvard. You know, that school that people (who matriculated) refer to obliquely: "Yeah, I went to school in Boston,” they will say. Like they're hoping we think it was Tufts and not embarrass them further. This might be the most important difference between Harvard and Yale—other than Yale being a second-rate school3—nobody gets to say “I went to school in New Haven” and have people get on with their day unaware of their Ivy League institution.
Harvard is more than just an ivory tower for the privileged with the plausible deniability of other excellent-enough schools in the neighborhood; however, it's also a place that generates a tremendous amount of medical science.
Today, the rocket ship that is “lesion-network mapping” (previously reviewed in this article) drops another booster as it smoothly moves into the stratosphere. First author Samantha Baldi and senior author Shan Siqqiqi took the trouble of looking at a large-scale data set out of McLean Hospital, evaluating the outcomes of depression treatment in individuals treated with H1 coil systems for depression, who had associated MRI scans.4 These were not fMRI—they were structural MRI scans. They had to perform complex math to back-solve for the brain circuits they know are present from prior research.
This circuit was significantly similar to a predefined causal depression circuit (spatial r = 0.59, p = 0.04) derived from TMS, deep brain stimulation, and lesion studies.
They were able to determine that the placement of those large coils, as it relates to engagement of the underlying depression brain circuit he has hypothesized, is highly correlated with response to dTMS treatment.
I am going to say that again without the “scientific hedging.”
It matters where you put the coil, based on the underlying brain network. If you engage the depression network, by putting the coil in the right spot, people get better-er.
Let's take a look at the data:
They evaluated modeled e-fields (the amount of brain engaged by the TMS coil) and evaluated if it would overlap with the brain circuit for depression as defined from prior data, and if those correlated with people getting better with the treatment:
E-fields with greater connectivity similarity to this circuit led to greater symptom improvement (r = 0.41, p < 0.001).
Lo and Behold: the more the circuit was engaged by the coil as placed, the more improvement occurred. It also appeared that, on average, the FDA label (which says “move the coil 6cm forward” isn’t actually in keeping with the best outcomes in every case:
Post-hoc analyses revealed that more posterior coil positioning increases H1 E-field overlap with the depression circuit, with high overlap at scalp locations 3–6 cm anterior to the motor hotspot. Thus, H1 coil stimulation sites that improve depression converge on a common causal depression circuit.
This is retrospective data, and it is not able to determine causally the same things we can from prospective and randomized designs, as the authors remind us:
Prospective studies are needed to validate these findings.
All of that being said…why does this complex science matter?
We learned just the other day that the largest accelerated TMS trial of all time was concluded—you know, the study I was an investigator on. The results were among the best results ever in a depression study:
The efficacy results are particularly impressive, with the accelerated protocol achieving 87.8% response and 78.0% remission rates
What Shan’s data suggest is that we can do even better if we place these coils in just the right spot. It is also plausible that this coil placement could be determined for H-coils at a lower cost and with more available structural MRI options versus expensive fMRI. There is more hope for depression than ever, thanks to science.
More work needs to be done, but depression may be a solved problem for the vast majority of people shortly, if only insurance keeps up.
Greetings, if you (or a loved one) are looking for relief from depression, OCD, anxiety, PTSD, Bipolar Disorder, or other conditions, feel free to explore care with Radial—it’s the company of which I’m a co-founder, delivering the most advanced mental health care on earth. If you are looking for help, Radial offers the most advanced mental health care.
Cole EJ, Phillips AL, Bentzley BS, Stimpson KH, Nejad R, Barmak F, Veerapal C, Khan N, Cherian K, Felber E, Brown R, Choi E, King S, Pankow H, Bishop JH, Azeez A, Coetzee J, Rapier R, Odenwald N, Carreon D, Hawkins J, Chang M, Keller J, Raj K, DeBattista C, Jo B, Espil FM, Schatzberg AF, Sudheimer KD, Williams NR. Stanford Neuromodulation Therapy (SNT): A Double-Blind Randomized Controlled Trial. Am J Psychiatry. 2022 Feb;179(2):132-141. doi: 10.1176/appi.ajp.2021.20101429. Epub 2021 Oct 29. PMID: 34711062.
SAINT is the brand name for the treatment delivered in the SNT trial.
I didn't attend either Harvard or Yale, but I think it’s fun to poke fun at them both.
Baldi, S., Chiulli, N., Palm, S. et al. Targeting depression circuitry with H1 coil Transcranial Magnetic Stimulation: a retrospective circuit mapping study. Neuropsychopharmacol. (2025). https://doi.org/10.1038/s41386-025-02157-5




Thanks, I am trying to keep up; this helps.
Isn’t that in the Constitution — every American is free to poke fun at Harvard and Yale? 🙂🇺🇸