Accelerated dTMS in Alcohol Use Disorder and "Very Treatment Resistant" Depression
It's been a big week!
One of the endlessly painful experiences for those interested in research? It is how long it takes for any of that to get out in the world. It takes even longer for any research to translate into clinical practice. The average time from a scientific publication to integration into clinical practice is 17 years. That's far too long. One of the reasons I regularly explain to the captive audience of my readers what's going on in research is that I want everybody to have more facility with research publications. If you have some sense of what you're reading, it's easier to put it into practice for you, your family, your practice, or your friends. It might even make it to a patient sooner rather than later. Without further due, I have some pretty exciting data, some of which is thanks to teams, including your author. We're going to start with research. I had nothing to do with it but was excited to see it. Accelerated transcranial magnetic stimulation is a modality the readers of this publication are familiar with, and yesterday, Brainsway published a pilot study on the use of aTMS in alcohol use disorder (AUD):
Six individuals—veterans all—were treated in an acute AUD treatment setting (residential) using the H7 coil:
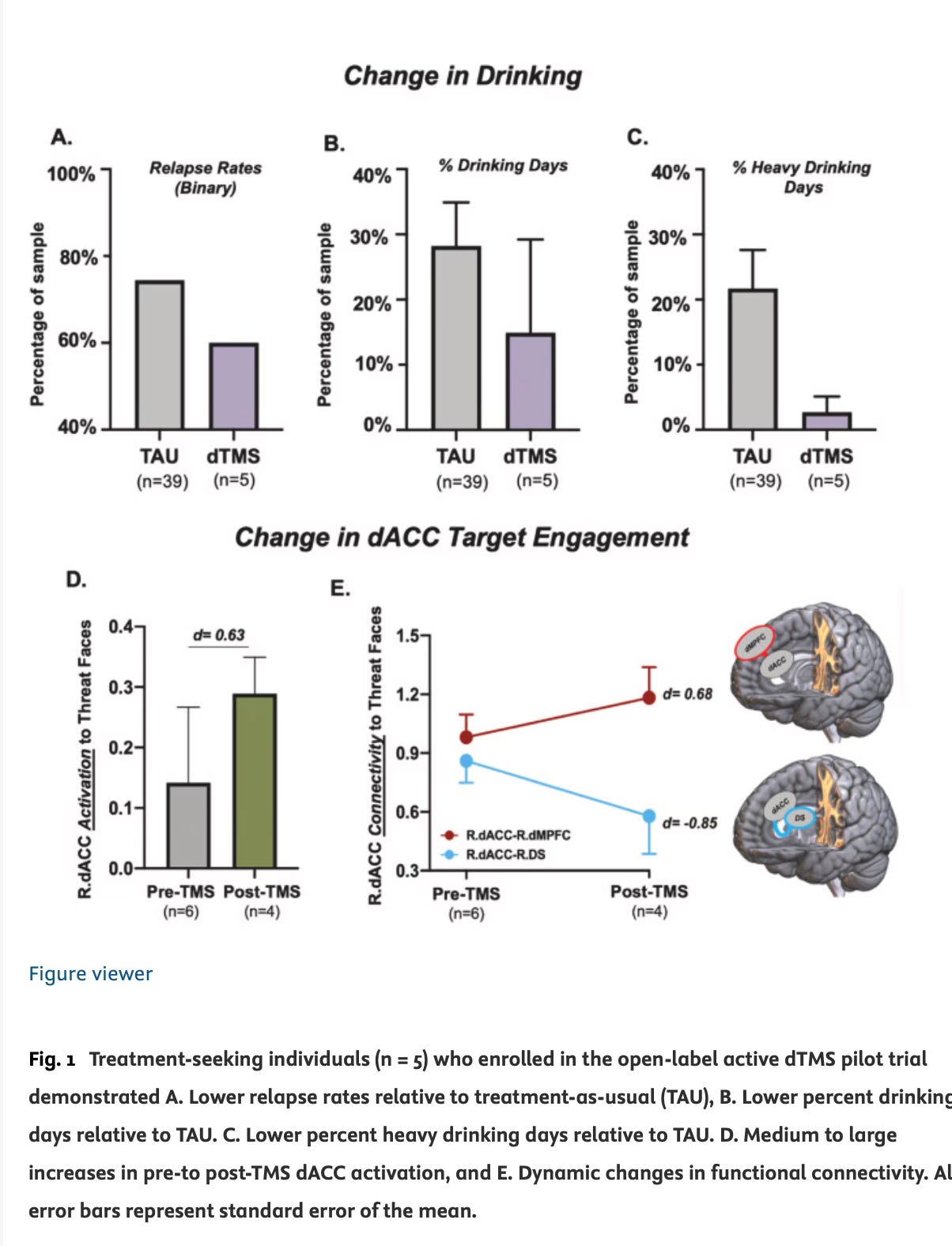
Alcohol relapse rates were reduced 6-months post-treatment following dTMS (60 %) compared to treatment-as-usual (74.4 %). In the last 90 days of the follow-up period (3mo–6mo post-treatment), there were fewer percent drinking days (dTMS: 14.9 ± 14.3 %, TAU: 28.2 ± 6.7 %) and heavy drinking days (dTMS: 2.7 ± 2.4 %; TAU: 21.7 ± 5.9 %) in the dTMS group compared to TAU.1
The helpful graphic is here:
In fairness, this wasn’t as accelerated as I would have done—it’s only three treatments a day, over 10 days, for a total of 30 treatments, over “10 consecutive business days.”
Aside from that, if I can do anything in my life, it's to advocate for business days no longer being a meaningful concept when it comes to healthcare treatment. Hospitals don't limit surgery to business days, and urgent or emergency outpatient mental health treatment shouldn't be limited to business days either.
Moving on to other science updates, the following comes out of my shop—Fermata—in Brooklyn, NY, in collaboration with the brilliant Dr. Irfan Handoo in Kansas City. These are all published open source in the new Journal “Transcranial Magnetic Stimulation.” What happens to people who are very, very treatment-refractory when it comes to depression? Can they still get better? Our answer to that question was to look for people who had not had successful responses to either rTMS and ketamine and ECT. If these individuals had gotten no benefit from the other best available treatments, was there still hope? Looking at our data utilizing deep transcranial magnetic stimulation—the H coils from Brainsway, above, we found that there was real hope for relief for many of these patients:
Methods: Six highly comorbid TRD patients were minimally responsive to “last line” treatment options (ECT, rTMS, IV Ketamine (IVK)) with (n=2) non-responders to rTMS + IVK and (n=4) unsatisfactory response to rTMS + ECT + IVK. All patients received dTMS with either H1 (n=5) or H7 (n=1) coil treatment. Patients (n=5) received either a high frequency protocol 10hz targeting L-DLPFC 1x for 36-40 days and patient (n=1) received 1800 pulses accelerated iTBS 10x for 5 days. Treatment evaluation was determined by PHQ-9.
Results: Patients presented baseline mean PHQ-9 scores of 23.83. Prior treatment had led to only partial response, resulting in 1.33% mean reduction with a range of 0% to 12.39%. Following dTMS treatment, there was an mean remission rate of 69.05%, (symptoms reduction mean, 61.74%; range 29.57%-100%). One patient experienced complete remission from depression. Post-treatment assessment was measured between 15-17 days after dTMS was concluded.2
My science update of the day? There's more coming every day and more hope — we're trying to make it more accessible, too.
Thank you for reading, and please feel free to share with your friends and colleagues.
Accelerated deep TMS in alcohol use disorder: A preliminary pilot trial targeting the dorsal anterior cingulate cortex increases neural target engagement and abstinence. Padula, Claudia B. et al. Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation, Volume 17, Issue 5, 1098 - 1100
Amna Aslam, Irfan Handoo, Carlene MacMillan, Owen Muir, SUCCESSFUL DTMS IN RTMS, ECT, AND KETAMINE REFRACTORY DEPRESSION: A CASE SERIES, Transcranial Magnetic Stimulation, Volume 1, 2024, 100043, ISSN 3050-5291, https://doi.org/10.1016/j.transm.2024.100043.