Pre-Payment Review: Do We Have Our First New Mental Health Parity Test Case?
United healthcare's policy of "deciding not pay" is an enforcement opportunity
I’m on a ✈️. It’s the AACAP annual meeting week in Seattle. That is the American Academy of Child and Adolescent Psychiatry. You know, the medical specialists who are very hard to access because many of them are either full, out of network, or both:
While millions of young people suffer from severe mental illnesses, there are only about 6,300 child and adolescent psychiatrists practicing in the United States. There is also a severe maldistribution of child and adolescent psychiatrists, especially in rural and poor, urban areas where access is significantly reduced.1
How dire is the shortage?
The median wait time was 50 days (interquartile range = 29–81 days). In adjusted models, adolescents with Medicaid waited longer than those with private insurance, especially during the spring (geometric mean = 50.9 vs. 41.9 days; p = 0.02).2
Well, don't worry—that is a paper from 2015! It’s only gotten worse since then (this is data from 2023):
Altogether, 948 psychiatrists were sampled in New York, California, North Dakota, Virginia, and Wyoming. Overall contact information accuracy averaged 85.3%. Altogether, 18.5% of psychiatrists were available to see new patients with a significantly longer wait time for in-person than telepsychiatry appointments (median = 67.0 days vs median = 43.0 days, p < 0.01). The most frequent reason for unavailability was provider not taking new patients (53.9%). Mental health resources were unevenly distributed, favoring urban areas.3
If you have a PPO plan, you can just pay for an out-of-network child psychiatrist and submit the claim for insurance reimbursement. You know, where they pay 70% of “reasonable and customary?” Otherwise, it is what the insurance company thinks the visit should cost. Except even that isn’t realistic anymore if you have United Healthcare. A policy—which they claim to have discontinued despite ample evidence to the contrary—called “pre-payment review” is the newest barrier to care. There is a legal name for this kind of discrimination in mental health care! It’s called an NQTL—a spicy acronym, I know.
As I previously put it: Nonquantitive Treatment Limitations (NQTLs) are the Cheating Boyfriends of Labor and Tax Law
Recently, the Biden administration’s Department of Labor issued a much stricter final rule on mental health parity. Lisa A. Gomez, the assistant secretary for Labor was interviewed by my friend and colleague Jeanne Pinder on the topic of if pre-payment review would be illegal.
“The question of whether or not it’s legal really depends on whether the insurance companies are asking for similar types of information if you are having a medical or surgical procedure rather than mental health,” she said.
“If a plan can say, ’if a person has a certain mental health condition or addiction, and then they have a medical condition that is similar within the same type of classification, and we make them jump through all of these hoops,’ then it’s fine. But the chances are very unlikely that they are requiring the same of both. That’s where it becomes a violation of the law.
It would have been more concise but less official-sounding to snort the water she was drinking and say, “Bro, it’s mad sus.” Then again, she is not my 8-year-old son.
It’s so “mad sus” that both the American Psychological Association and the American Psychiatric Association have come together, issuing a rare APA^2 statement:
“Under the HIPAA minimum necessary rule (45 CFR § 164.502(b)), Optum is obligated to seek only the minimum information necessary to accomplish the purpose for which information is sought,” the letter says. “The fact that Optum has for years been able to process [out of network] mental health claims without the extensive patient documentation it now requires before payment is a strong indication that such extensive documentation is not, in fact, necessary.”
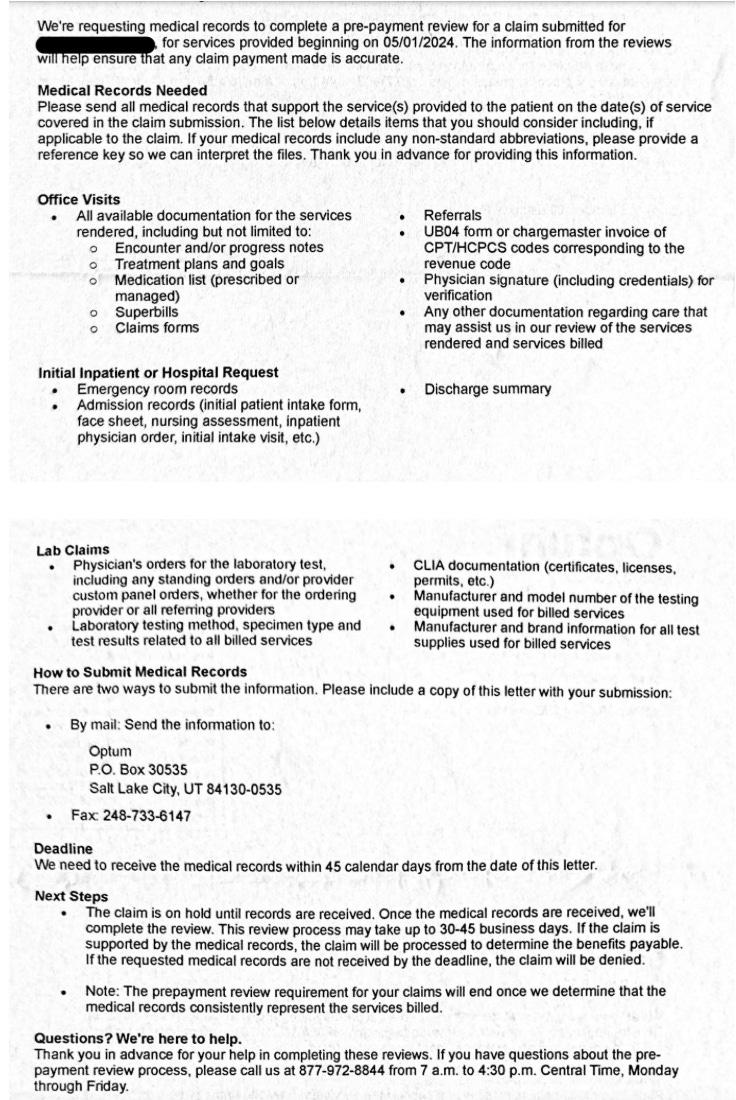
Optum, part of United Healthcare, has been requesting unbelievable mountains of data before it pays providers or families for claims, in or out of network:
The documents Optum requested in its PPR letter include, for each claim: “Encounter and/or progress notes, treatment plans and goals, medication list (prescribed or managed), superbills, claims forms, referrals, UB04 form or chargemaster invoice of CPT/HCPCS codes corresponding to the revenue code, physician signature (including credentials) for verification, any other documentation regarding care that may assist us in our review of the services rendered and services billed,” as well as any hospital records.
Also requested: “Lab claims: Physician’s orders for the laboratory test, including any standing orders and/or provider custom panel orders, whether for the ordering provider or all referring providers, laboratory testing method, specimen type and test results related to all billed services, CLIA documentation (certificates, licenses, permits, etc.), manufacturer and model number of the testing equipment used for billed services, manufacturer and brand information for all test supplies used for billed services.”
Which— I think we can all agree— is a bit much when it comes to data to support paying a $300 bill for a therapy session. How was that blood work going to change management?
This is a mountain of very private data being demanded by the same security geniuses who didn't bother to use 2FA on any of our data when they allowed themselves to be extorted by RansomHub and/or BlackCat earlier this year:
A few days later, the Brooklyn psychiatrist Owen Muir expanded the joke into an extended transcript of a satirical “all-hands town hall” in which ALPHV, the Russia-based ransomware group that had taken credit for breaching Change, explains to angry stakeholders why the operation is taking so long: After days of “having to say representative, over and over again,” they finally learned they needed to submit their ransom request via fax machine, at which point they learned that they needed to wait 14 days for a peer review with one of UnitedHealth’s in-house hackers, to “determine if our ransom request is … How do they put it? Oh, reasonable and customary.”
“It turns out their whole business is structured around ‘ransom requests,’ except it’s not for the data, it’s for human health,” the “hacker” observes.
So, given United Healthcare admitted to violating the Mental Health Parity Law in New York in 2021, which means they agree they are responsible for complying with the law, it seems it might be the basis for yet more litigation to be at it all over again?
United Behavioral Health and United Healthcare Insurance Co. will pay $13.6 million to affected participants and beneficiaries; pay $2,084,249 in penalties; and take other corrective actions following investigations and litigation by the U.S. Department of Labor and the New York State Attorney General.
Corrective action? It was not violating parity law…Hard Enough—United: the “Diddy Party” approach to health benefits compliance?
Follow ClearHealthCosts.com for more. It provides exceptional reporting, unlike some other outlet I could name in a legal filing. Oh, wait. I did, in bullet points 19, 20, 21, 22, 23, and 24, of testimony under penalty of perjury.
Kim, W. J., & American Academy of Child and Adolescent Psychiatry Task Force on Workforce Needs. (2003). Child and adolescent psychiatry workforce: a critical shortage and national challenge. Academic Psychiatry, 27(4), 277-282.
Steinman, K. J., Shoben, A. B., Dembe, A. E., & Kelleher, K. J. (2015). How long do adolescents wait for psychiatry appointments?. Community mental health journal, 51, 782-789.
Sun, C., Correll, C. U., Trestman, R. L., Lin, Y., Xie, H., Hankey, M. S., Uymatiao, R. P., Patel, R. T., Metsutnan, V. L., McDaid, E. C., Saha, A., Kuo, C., Lewis, P., Bhatt, S. H., Lipphard, L. E., & Kablinger, A. S. (2023). Low availability, long wait times, and high geographic disparity of psychiatric outpatient care in the US. General Hospital Psychiatry, 84, 12-17. https://doi.org/10.1016/j.genhosppsych.2023.05.012



Wait time for services in rural areas might be closer to infinity than the stated average. People who are denied access do not have a wait time after all .
I can't believe Optum's letter.
Not just mad sus. Super strong Ohio vibes. 🙂